One-stage autotransplantation of a third molar with unformed roots in an adolescent. Clinical case
Downloads
Abstract
The first permanent molars in children are most often affected by decay, resulting in their early loss. Autografting of teeth, particularly the third molar, can be an alternative to dental implantation or prosthetic treatment. This technique has long been used in adult patients, but is not widely used in children. The goal is to estimate the effectiveness of the method of one-stage autotransplantation of third molars with unformed root in the place of the extracted first molars in adolescents.Materials and methods.
A clinical case of one-stage autotransplantation of the 4.8 tooth in the place of the extracted 4.6 tooth in a 16-year-old female patient is described. X-ray diagnosis and short-term orthodontic treatment were performed beforehand to create a place for the recipient tooth. Surgery was performed on an outpatient basis, under local anesthesia. A similar operation followed six months later: a one-stage autografting of a more anatomically suitable tooth 2.8 in place of the extracted tooth 1.6.
Results.
Positive results of treatment were obtained in 2 years of observation: formation of the third molar roots was completed in the recipient's bed, the periodontal gap was formed.
Conclusion.
Autografting of teeth is an accessible and minor traumatic method of one-stage replacement of dystopian or retained third molars with unformed roots of extracted molar or premolar (depending on the size), which can be used in adolescents in case of early removal of destroyed permanent teeth. This technique is very successful and predictable if the indications and conditions are met, but it requires continuous monitoring until the root system is complete.
Key words:
autotransplantation of teeth, third molar with unformed roots, childrenFor Citation
Introduction
The first permanent molars are most susceptible to caries for several reasons. As one of the first permanent teeth in the mouth, they often appear unnoticed by parents and a child. Furthermore, the hygiene of these teeth is difficult because of a child's poor manual skills. The rapid development of dental caries in these teeth is provoked by immature and less mineralized enamel [1]. According to data, over 50% of children under the age of twelve have first permanent molars affected by caries, that subsequently leads to the early loss of these teeth and dental deformities or anomalies of the dentition [2]. Unfortunately, dentists cannot replace dental defects with implants or orthopedic constructions until the age of 18, so as an alternative to implantation in adolescents, the technique of transplanting third molars buds into the post-extraction alveolus of molars or premolars can be suggested [3, 4].
Dental autotransplantation is a method of restoring the integrity of the dentition, which is most often used in the case of a therapeutic molar or premolar extraction while a third molar with formed or unformed roots is available. The method is characterized by a short period of wound healing and prompt rehabilitation. In comparison with the implant method of treatment, a transplanted tooth retains proprioception due to the restoration of periodontium and periodontal ligament [5—9].
Indications for autotransplantation of teeth are: the loss of a tooth due to the complications of caries or traumatic affections, and also primary adentia of a permanent tooth in the presence of a temporary tooth.
The technique has shown high efficiency. According to scientific literature, the survival rate of autotransplanted teeth with unformed roots is 95% and with formed roots — 90.5—98% [10]. The complications of the procedure may include a replacement resorption, ankylosis, pathological mobility and loss of the transplanted tooth [11]. Favorable prognostic factors for this technique are: young age of patients (15—25 years), possibility of atraumatic extraction, enabling condition of the recipient area, periodontal ligament on both sides of the wound [12, 13]. At the same time, optimal adaptation of the periodontal ligament is demonstrated when the tooth is moved directly into the recipient socket [14, 15]. It is important to note that the optimal third molar root length should be from 2/3 to the full length of the formed tooth [16].
Criteria for evaluating the success of autotransplantation:
- Apexogenesis and apexification — the length from the given points (medial and distal roots from the enamel-cement border to the most apical point) was determined on the targeted radiographs.
- Temperature test — based on the movement of fluid in the dentinal tubules. Exposure to a cold stimulus causes fluid shifts in the lumen of the tubules, which irritates the peripheral pulp tissue.
- Local bone repair space — the gap between the root surface and the alveolus, assessed radiologically and clinically.
Factors negatively affecting a one-stage autotransplantation of third molars:
- Extraoral time should not exceed 15 minutes.
- Traumatic damage to the ligament apparatus of the donor tooth during the extraction of the tooth, its insertion into the recipient site.
- Holding the tooth outside the oral cavity in a non-humid environment.
A literature search on the use of this technique in children, with the key words “Tooth autotransplantation” and “children”, over the past 5 years on the PubMed resource resulted in 35 articles. The Russian resource eLibrary.ru found 1 article in the last 10 years. The search results suggest that the technique of dental autotransplantation in children in Russia is not widespread enough, while in the world practice it is being actively studied and improved.
A clinical case of a successful one-stage implantation of a dystopian third molar with unformed roots into the post-extraction socket of the first molar in the maxilla and mandibula is represented bellow.
Clinical case
In January 2019, a 16-year-old patient and her parents went to the dental clinic of the Kuban State Medical University for the removal of the right mandibular first molar. The patient complained of a defect in the artificial crown of tooth 4.6.
Tooth 4.6 was previously treated for caries complications; the patient was referred by the pediatric dentist of the municipal polyclinic for extraction of tooth 4.6 due to the exacerbation of chronic periodontitis. The patient had previously had tooth 3.6 extracted for caries complications.
Objectively: facial configuration is unchanged, skin and visible mucosa are clean, regional lymph nodes are not palpated, lip closure is correct, mouth opening is full, painless, masticatory muscles are painless on palpation, turgor is preserved. In the mouth: mucosa is pale pink, moist; neutral occlusion; tooth 4.6 is covered with a metal-ceramic crown, marginal fit of which is unsatisfactory, percussion of the tooth is positive, grade 1 tooth mobility, marginal gingiva in the area of tooth 4.6 is hyperemic, edematous, bleeding when probing, alveolar gingiva in the area of 4.6 is slightly hyperemic, painless.
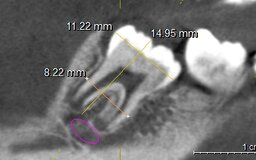
Computed tomography (CT) of the mandible (Fig. 1) shows an area of bone tissue destruction in the apexes of tooth 4.6, rounded shape with clear boundaries (Fig. 2). Besides, the formed right mandibular third molar bud in the stage of root growth in length is visualized.
Based on the clinical data, examination, and CT scan analysis, chronic granulomatous periodontitis of tooth 4.6 in the exacerbation stage was diagnosed.
Out of several treatment options, the patient and her parents chose the procedure of autotransplantation of the third right molar into the post-extraction socket of the right mandibular first molar.
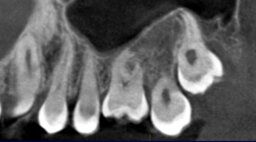
CT scan analysis increases the predictability of the treatment and gives an insight into possible healing patterns: the longitudinal and transverse dimensions of the transplanted tooth were determined and compared with the dimensions of the tooth to be extracted. On the basis of these data, it turned out that the donor tooth was larger than the recipient tooth in the mesiodistal direction (Fig. 3, 4).
In order to create space for the recipient tooth, it was decided that orthodontic preparation should be carried out: the metal-ceramic crown should be replaced with a temporary plastic crown with a spring for the distal inclination of tooth 4.7 (Fig. 5).
A month and a half later, tooth 4.7 shifted distally by the required 1.5 mm.
After antiseptic treatment under mandibular and infiltration anesthesia with 2.2 ml of Ultracaini DS forte (Sanofi Aventis, France), exodontia of the right mandibular first molar was performed, followed by curettage of the extraction site and antiseptic treatment with metronidazole. The cavity 4.6 was treated with a round cutter and the interradicular septum was removed for the passive insertion of the transplanted tooth. Tooth 4.8 was atraumatically removed (Fig. 6).
Tooth 4.8 was transplanted into the cavity of tooth 4.6. The transplanted tooth was splinted with orthodontic wire to the adjacent teeth for 30 days (Fig. 7).
The cavity of tooth 4.8 was sutured with atraumatic floss, and the soft tissue around the transplanted tooth was also sutured, tightly covering the tooth.
Note that the transplanted tooth was being constantly held in a humid environment (sterile napkin moistened with NaCl solution + Metrogyl); extraoral time did not exceed 7 minutes, which allowed us to avoid any damage of the periodontal tissues, which were on the surface of the root of the transplanted tooth.
The dynamics of the tooth 4.8 root formation was assessed radiologically immediately after surgery, as well as 3 and 6 months after (Table 1, Fig. 8, 9, 10).
| The root length (mm) | ||
| medial | distal | |
| Immediately after surgery (Fig. 8) | 8.7 | 8.2 |
| After 3 months (Fig. 9) | 8.8 | 8.3 |
| After 6 months (Fig. 10) | 9.5 | 8.8 |
A cotton ball soaked in ethyl chloride solution was used for the temperature test. The ball was placed on the middle third of the tooth crown and subjective reaction to the cold stimulus was evaluated (Table 2).
| Observation period | Reaction to a stimulus |
| Immediately after surgery | not present |
| After 3 months | not present |
| After 6 months | weakly positive |
| After 12 months | positive |
Bone density in the mediodistal, vertical, and vestibulo-lingual positions was determined on targeted radiographs. Clinically, this was determined by the condition of the periodontal bone tissue and the depth of the periodontal sulcus.
The result of tooth 4.8 transplantation two years after the surgery is shown in Fig. 11.
In August 2019, the patient was offered an extraction of the destroyed tooth 1.6 with a one-stage autotransplantation of the third molar. After obtaining consent from the patient and parents, preparations for surgical treatment began. Objectively: facial configuration is unchanged, skin and visible mucosa are clean, regional lymph nodes are not palpated, lip closure is correct, mouth opening is full, painless, masticatory muscles are painless on palpation, turgor is preserved. In the mouth: mucosa is pale pink, moist; neutral occlusion; previously treated for caries complications tooth 1.6 is destroyed, percussion of the tooth is painless, no mobility, marginal gingiva in the area of tooth 1.6 bleeds when probing (Fig. 12).
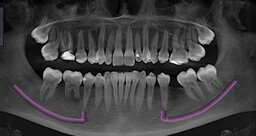
A CT scan analysis revealed chronic periodontitis of tooth 1.6 (apical parts of tooth 1.6 had cysts), and the difference between the sizes of teeth 1.8 and 1.6, so an impacted tooth 2.8, close to tooth 1.6 in its anatomic size, with incomplete root formation was selected as a donor tooth (Fig. 13, 14, 15).
Surgical intervention was performed according to the above described methodology: antiseptic treatment, infiltration anesthesia 1.8 ml of Ultracaini DS forte (Sanofi Aventis, France), exodontia of the mandibular right first molar was followed by curettage of the cavity and antiseptic treatment with metronidazole. The cavity 1.6 was also treated with a round cutter and the intercorneal septum was removed for passive insertion of the transplanted tooth. Then tooth 2.8 was removed atraumatically. The tooth was transplanted into the prepared extraction site of tooth 1.6, followed by splinting with orthodontic wire (Fig. 16).
One year after the operation the patient had no complaints. No pathological changes of the transplanted tooth and the oral mucosa in the recipient site were detected neither clinically in the oral cavity nor radiographically (Fig. 17, 18).
Two years after the surgical intervention (February 2021), the patient underwent orthodontic treatment with a brace system. No contraindications for treatment were identified. The dental images of the transplanted teeth are shown below (Fig. 19, 20).
Conclusion
One-stage autotransplantation of the third molars with unformed root into the post-extraction socket of the first molar in the maxilla and mandibula was performed. The transplanted teeth were splinted to the adjacent teeth with orthodontic wire for 1 month. After 4 months, radiological examination revealed root growth in length, bone formation between the third molar and alveolus of the extracted tooth, formation of periodontal gap throughout the root. The autotransplanted teeth reacted positively to the cold stimulus, were immobile, the gingiva in the area of surgical intervention was physiologically colored without inflammatory symptoms.
Thus, autotransplantation of teeth is an affordable, high-quality and low-traumatic method of a one-stage replacement of the removed molar or premolar (depending on the size) by a dystopian or impacted third molar with unformed roots, which can be used in adolescents in the case of early removal of destroyed permanent teeth. This technique is very successful and predictable, if the indications and conditions are met, but it requires constant dynamic monitoring of these teeth until the root system is formed.
References
- Leous P.A., Kiselnikova L.P. Retrospective evaluation of dental caries trends and assessing the caries disease determinators in Moscow children. Paediatric dentistry and prophylaxis. 2016; 15 (2): 57—63 (In Russ.). eLIBRARY ID: 27178231
- Kuzmina E.M., Yanushevich O.O., Kuzmina I.N. Dental morbidity in the Russian population. Epidemiological dental examination of the population of Russia. Moscow: Moscow State University of Medicine and Dentistry, 2019. Pp. 13—25 (In Russ.).
- Badalyan V.A., Zedgenidze A.M. Tooth autotransplantation. Russian Journal of Dentistry. 2019; 23 (6): 263—9 (In Russ.). eLIBRARY ID: 42340163
- Nimčenko T., Omerca G., Bramanti E., Cervino G., Laino L., Cicciù M. Autogenous wisdom tooth transplantation: A case series with 6—9 months follow-up. Dent Res J (Isfahan). 2014; 11 (6): 705—10. PMID: 25540668
- Asif J.A., Noorani T.Y., Alam M.K. Tooth auto-transplantation: An alternative treatment. Bull Tokyo Dent Coll. 2017; 58 (1): 41—48. PMID: 28381733
- Kamadjaja D.B. Autogenous transplantation: an alternative to replace extracted tooth. Dental Journal. 2015; 48 (3): 139—143. DOI: 10.20473/j.djmkg.v48.i3.p139-143
- Zakershahrak M., Moshari A., Vatanpour M., Khalilak Z., Ara A.J. Autogenous Transplantation for Replacing a Hopeless Tooth. Iran Endod J. 2017; 12 (1): 124—7. PMID: 28179939
- Grisar K., Chaabouni D., Romero L.P.G., Vandendriessche T., Politis C., Jacobs R. Autogenous transalveolar transplantation of maxillary canines: a systematic review and meta-analysis. Eur J Orthod. 2018; 40 (6): 608—16. PMID: 29860316
- Plotino G., Sans F.A., Duggal M.S., Grande N.M., Krastl G., Nagendrababu V., Gambarini G. Clinical procedures and outcome of surgical extrusion, intentional replantation and tooth autotransplantation a narrative review. Int Endod J. 2020; 53 (12): 1636—52. PMID: 32869292
- Jakobsen C., Stokbro K., Kier-Swiatecka E., Ingerslev J., Thorn J.J. Autotransplantation of premolars: does surgeon experience matter?. Int J Oral Maxillofac Surg. 2018; 47 (12): 1604—1608. PMID: 30170776
- Martin K., Nathwani S., Bunyan R. Autotransplantation of teeth: an evidence-based approach. Br Dent J. 2018; 224 (11): 861—864. PMID: 29855592
- Slivkin A.A., Fedotova E.A., Iordanishvili A.K., Guk V.A., Melnikov M.V. Autologous transplantation of wisdom teeth. Russian Military Medical Academy Reports. 2020; 39 (S3—5): 152—6 (In Russ.). eLIBRARY ID: 44386318
- Ong D., Itskovich Y., Dance G. Autotransplantation: a viable treatment option for adolescent patients with significantly compromised teeth. Aust Dent J. 2016; 61 (4): 396—407. PMID: 27029674
- Rohof E.C.M., Kerdijk W., Jansma J., Livas C., Ren Y. Autotransplantation of teeth with incomplete root formation: a systematic review and meta-analysis. Clin Oral Investig. 2018; 22 (4): 1613—1624. PMID: 29525924
- Tsukiboshi M., Yamauchi N., Tsukiboshi Y. Long-term outcomes of autotransplantation of teeth: A case series. Dent Traumatol. 2019; 35 (6): 358—67. PMID: 31127697
- Rohof E.C.M., Kerdijk W., Jansma J., Livas C., Ren Y. Autotransplantation of teeth with incomplete root formation: a systematic review and meta-analysis. Clin Oral Investig. 2018; 22 (4): 1613—24. PMID: 29525924