DOI:
10.37988/1811-153X_2021_1_150Evaluation of the precision of CAD/CAM-fabricated dental implant-supported bar systems
Downloads
Abstract
According to Branemark P.I. the level of possible micro-gap between the implant and the orthopedic construction should not exceed 10 microns. For cast bar constructions on implants, the level of micro-gap between the implant and the orthopedic construction has values of 390±70 microns for the cobalt-chromium alloy and 800±40 microns for the titanium alloy, which requires the use of additional technologies for correction. In order to improve the precision of bar constructions on implants, milling of solid blocks of various materials is used according to the CAD/CAM method.Material and methods.
The precision of the bar constructions made using CAD/CAM systems based on dental implants was evaluated depending on the material used and the number of support implants. 20 bar constructions on 4, 6 supports made of titanium and cobalt-chrome alloy were manufactured using milling machines of 5-axis CAD/CAM systems.
Results.
All manufactured bar constructions supported by dental implants showed acceptable values of micro-gap in the field of dental implant analogues in the laboratory model, regardless of the material used and the number of support implants.
Conclusions.
The production of bar constructions supported by dental implants by milling them using 5-axis CAD/CAM systems can be recommended as a method of choice in the orthopedic treatment of patients with complete absence of teeth.
Key words:
bar construction on dental implants, CAD/CAM, titanium alloy, cobalt-chromium alloyFor Citation
INTRODUCTION
Modern dentistry provides dental patients with a variety of treatment options not available in the recent past. With the use of dental implants, you can create additional supports for orthopedic structures. Classic full removable dentures with soft tissue support in the lower jaw have many drawbacks and hardly provide the functions assigned to them, especially with significant atrophy. So, this type of prosthesis can be displaced in the oral cavity at a distance of more than 10 mm, in particular when the maxillary-hyoid and buccal muscles contract during chewing food or speech, forming unstable occlusal contacts [1]. The main complaints include the mobility of the prosthesis, pain when chewing, impaired diction, unsatisfactory appearance of the prosthesis, difficulty in eating. There is a difference in proprioceptive activity with different orthopedic constructions. Patients with natural teeth feel a gap between teeth of 20 µm, with implants - at 50 µm, and with full removable dentures - at 100 µm [2]. Patients with complete absence of teeth have a reduced psychosocial status even in the case of good adaptation to a traditional removable denture [3]. When comparing the methods of orthopedic treatment of patients with complete absence of teeth in the lower jaw with classical removable and implant-supported prostheses, there is a higher level of patient satisfaction in the case of choosing the latter [4]. Also, when prosthetics with full prostheses on implants, there is a higher functionality in the seizure and chewing of food, as well as a decrease in pain and discomfort indicators, an increase in the ability to lead a more active and social lifestyle [5, 6]. Prosthetics with the use of implants in patients with complete absence of teeth improves neuromuscular activity and adaptation, improving chewing function [7]. A special group is made up of bar constructions on implants with a counter-bar in the prosthesis [8]. The prosthesis rests on implants splinted by a bar in the anterior region and on the mucous membrane in the posterior region of the jaw. Under the action of vertical loads, the implants perform the function of a prosthetic bed; in the distal part, the pressure is distributed over the mucous membrane. Retention in this group of prostheses counteracts lateral and overturning movements. The advantages of removable structures on implants include the possibility of easier hygienic manipulations by the patient in comparison with fixed structures. Also, removable constructions on implants in the absence of teeth can have more voluminous lip flanges and create a favorable aesthetic effect by supporting soft tissues. The disadvantages include the psychological aspect and progressive tissue atrophy under the prosthesis. One of the most important factors in the success of orthopedic treatment with the use of dental implants is the accuracy of the fit of the manufactured orthopedic structure [9]. Mechanical and biological complications are the result of inadequate fit of the prosthetic structure on the implants. The most common mechanical complications include loosening or fracture of a prosthetic screw, fracture of an abutment or prosthesis. In addition, the micro-gap between the implant and the prosthesis can be colonized by bacteria, which, in turn, can contribute to the destruction of peri-implant tissues [10]. Studies have been conducted on the effect of different levels of deformity on bone tissue. At the same time, it was noted that bone tissue is prone to fracture in the presence of 1–2% deformity, and in the presence of 2–40% deformation, bone tissue lysis or the formation of fibrous tissue in the area subject to stress occurs [11]. One of the first to formulate the theory of bone remodeling from the influence of stress was Kummer [12].With an increase in deformity above physiological limits, microfractures of bone tissue and resorption are possible. Violation of the trophism of bone tissue due to compression can also lead to its lysis and expose this zone to an increased destructive effect of anaerobic bacteria. Thus, until the value of the permissible inaccuracy has been determined, clinicians should strive to maximize the accuracy of the fit of orthopedic structures in order to reduce the risk of the negative influence of force factors and the appearance of possible complications. The Sheffield test is used to determine the accuracy of the fit of an orthopedic construction on implants in clinical and laboratory conditions [13]. This test is performed on one-piece prosthetics supported by multiple implants. The technique is as follows: if, when the structure is seated and the screw of one of the most distal implants is tightened, there is no significant gap between the structure and the rest of the implants, it is considered clinically acceptable. To measure the micro-gap, digital microscopy and a special impression material are used. Measurements by digital microscopy are made at the implant / prosthetic connection points [14], the values obtained are measured in micrometers. A special impression material is placed between the prosthetic construction and the implant, then its thickness is measured. This technique has not gained popularity due to inaccuracy and a large number of errors. Unlike natural teeth, which normally can have mobility in the holes due to the mobility of the ligament, the micromobility of the implant is represented by minimal values [15]. Consequently, errors in orthopedic treatment with implants can lead to a higher risk of complications. When studying the accuracy of fit of cast beam structures on implants, the edge gap was studied using digital microscopy. For cast bar constructions on implants, the level of the micro-gap between the implant and the prosthetic structure is 390 ± 70 µm for the cobalt-chromium alloy and 800 ± 40 µm for titanium, which requires the use of additional technologies for correction [16]. To date, to improve the precision of various orthopedic structures, including bar structures on implants, CAD / CAM milling is used from solid blocks of various materials [17–23]. Depending on the number of abutment implants and the material used for cast bar structures, the fit is well understood, but in the case of CAD / CAM milling, this relationship is not well understood for this type of structure. Therefore, a comparative analysis of the accuracy of fit of CAD / CAM-based bar constructions based on dental implants is relevant and useful for determining the optimal manufacturing technique for this type of structures, improving the quality and predicting long-term results of orthopedic treatment of patients.
The aim of the study was to evaluate the precision of CAD / CAM-milled bar constructions with support on dental implants, manufactured for orthopedic treatment of patients, depending on the material used and the number of supporting implants.
MATERIALS AND METHODS
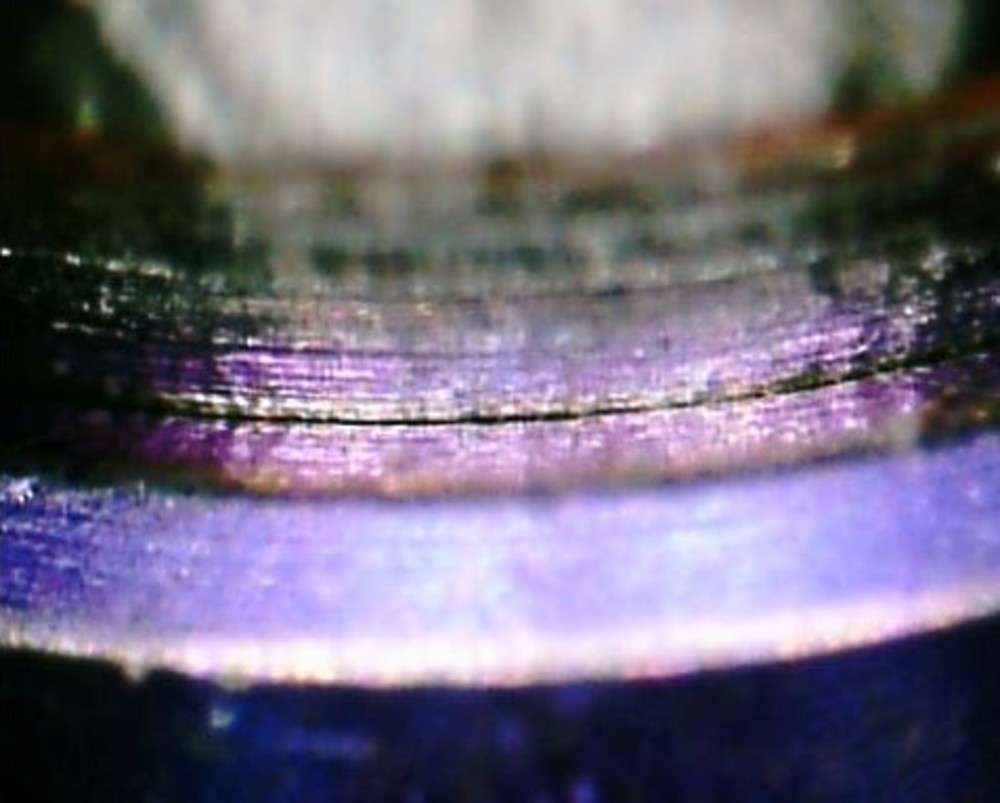
Comprehensive examination and treatment of patients with complete absence of teeth in the lower jaw was carried out on the basis of the Central research institute of dental and maxillofacial surgery (Moscow, Russia) and Private Clinics of the Moscow Region from 2017 to 2020, inclusive. A total of 20 people were examined - 12 women and 8 men from 35 to 77 years old, with pre-installed 4 or 6 dental implants on the lower jaw. On 5-axis milling machines using CAD / CAM systems, 20 bar constructions were made on 4 or 6 supports from titanium or cobalt-chromium alloy (Fig. 1, 2). The total number of supporting implants is 100. The method of digital microscopy was used to determine the accuracy of the fit of bar constructions on analogs of dental implants. The measurements were carried out according to the Sheffield method. The micro-gap that occurs when the fixing screw is tightened from the opposite side of the construction between the end support analog of the dental implant and the bar construction was measured. For fixation, a torque wrench with a torque of 25 Ncm was used. The study was carried out from the vestibular surface, perpendicular to the connection of the implant analog with the bar structure (Fig. 3). Images obtained with a digital microscope were scaled using the MicroCapture program. The average value of the micro-gap was measured in micrometers, and the measurement accuracy was assessed. A comparative analysis of measurements taken before and after tightening all screws of the bar construction was carried out. Table 1 shows the results of a statistical analysis of the comparison of the characteristics of bar constructions depending on the number of supporting implants.The objectives of this analysis are to test the null statistical hypothesis about the equality of distributions in groups, as well as to identify those indicators for which the null hypothesis is rejected in favor of the alternative, with confirmation of the presence of statistically significant differences between the groups. For comparison in terms of quantitative indicators, the nonparametric Mann-Whitney test is used, and for comparison in terms of binary and nominal indicators, the Pearson χ2 test is used. As follows from the table. 1, statistically significant differences between installation on 4 or 6 implants were found only in the accuracy of the Sheffield test - 1.57 ± 0.26 versus 1.27 ± 0.18 μm (p = 0.0095). The statistically processed data on the magnitude of microgaps obtained from the results of digital microscopy in the area of contact zones of analogs of dental implants and milled bar constructions, depending on the material used for the manufacture of the bar constructions, are presented in Table. 2. According to P.I. Branemark, the possible micro-gap between the implant and the prosthetic structure should not exceed 10 µm [24]. Based on the results of this study, acceptable values of the micro-gap in the area of contact between implants and milled bar structures were obtained. Milling using CAD / CAM systems made it possible to obtain high-precision bar constructions supported on dental implants, regardless of the number of supporting implants (4 or 6) and the material used (titanium or cobalt chromium alloy).
CONCLUSIONS
According to the data obtained in the course of the study, the following clinical recommendations can be formulated for the manufacture of a bar constructions based on dental implants:
- Both titanium and cobalt-chromium alloy can serve as a material.
- For prosthetics on both 4 and 6 dental implants, CAD / CAM milling allows for the production of high-precision constructions.
- Milling using CAD / CAM systems allows to obtain constructions with consistently acceptable accuracy.
Thus, the manufacture of bar constructions based on dental implants on 5-axis milling machines can be recommended as the method of choice in the orthopedic treatment of patients with complete absence of teeth.
Table 1. Comparison of the bar constructions according to the number of supporting implants
|
Indicator |
Number of supports |
p |
|
|
4 (n=10) |
6 (n=10) |
||
|
Patient data |
|||
|
Age, years |
57,20±14,05 |
52,10±10,32 |
0,4958 |
|
Data of fit |
|||
|
Passive fit, μm |
7,48±0,81 |
6,98±0,62 |
0,1736 |
|
Passive fit accuracy, μm |
1,55±0,49 |
1,45±0,27 |
0,8480 |
|
Sheffield test, μm |
6,79±1,04 |
7,17±0,99 |
0,4057 |
|
Sheffield Test Accuracy, μm |
1,57±0,26 |
1,27±0,18 |
0,0095 |
|
Complete tightening of all |
6,68±0,90 |
6,91±1,06 |
0,5202 |
|
Accuracy of full tightening of all screws, μm |
1,53±0,35 |
1,56±0,32 |
0,8194 |
Table 2. Comparison of the bar constructions according to the alloy
|
Indicator |
Material |
p |
|
|
Ti (n=10) |
Co-Cr (n=10) |
||
|
Patient data |
|||
|
Age, years |
59,60±13,00 |
49,70±9,74 |
0,1208 |
|
Data of fit |
|||
|
Passive fit, μm |
7,02±0,67 |
7,44±0,79 |
0,1988 |
|
Passive fit accuracy, μm |
1,51±0,45 |
1,49±0,34 |
0,9389 |
|
Sheffield test, μm |
6,66±1,21 |
7,30±0,68 |
0,2265 |
|
Sheffield Test Accuracy, μm |
1,41±0,23 |
1,43±0,31 |
0,9392 |
|
Complete tightening of all |
6,52±0,97 |
7,07±0,92 |
0,2565 |
|
Accuracy of full tightening of all screws, μm |
1,56±0,38 |
1,53±0,28 |
0,9696 |


References
- Palmer J.B., Rudin N.J., Lara G., Crompton A.W. Coordination of mastication and swallowing. — Dysphagia. — 1992; 7 (4): 187—200. PMID: 1308667
- Boven G.C., Raghoebar G.M., Vissink A., Meijer H.J.A. Improving masticatory performance, bite force, nutritional state and patient›s satisfaction with implant overdentures: a systematic review of the literature. — J Oral Rehabil. — 2015; 42 (3): 220—33. PMID: 25307515
- Amaral C.F., Pinheiro M.A., de Moraes M., Garcia R.C.M.R. Psychometric analysis and masticatory efficiency of elderly people with single-implant overdentures. — Int J Oral Maxillofac Implants. — 2018; 33 (6): 1383—9. PMID: 30427971
- Mishra S.K., Chowdhary R. Patient›s oral health-related quality of life and satisfaction with implant supported overdentures -a systematic review. — J Oral Biol Craniofac Res. — 2019; 9 (4): 340—6. PMID: 31508300
- Sharma A.J., Nagrath R., Lahori M. A comparative evaluation of chewing efficiency, masticatory bite force, and patient satisfaction between conventional denture and implant-supported mandibular overdenture: An in vivo study. — J Indian Prosthodont Soc. — 2017; 17 (4): 361—72. PMID: 29249880
- Swelem A.A., Abdelnabi M.H. Attachment-retained removable prostheses: Patient satisfaction and quality of life assessment. — J Prosthet Dent. — 2020; S0022—3913 (20)30408-X. PMID: 32893014
- von der Gracht I., Derks A., Haselhuhn K., Wolfart S. EMG correlations of edentulous patients with implant overdentures and fixed dental prostheses compared to conventional complete dentures and dentates: a systematic review and meta-analysis. — Clin Oral Implants Res. — 2017; 28 (7): 765—73. PMID: 27302014
- Pozzi A., Tallarico M., Moy P.K. Four-implant overdenture fully supported by a CAD-CAM titanium bar: A single-cohort prospective 1-year preliminary study. — J Prosthet Dent. — 2016; 116 (4): 516—23. PMID: 27160781
- Şen N., Şermet I.B., Gürler N. Sealing capability and marginal fit of titanium versus zirconia abutments with different connection designs. — J Adv Prosthodont. — 2019; 11 (2): 105—11. PMID: 31080571
- Tsuruta K., Ayukawa Y., Matsuzaki T., Kihara M., Koyano K. The influence of implant-abutment connection on the screw loosening and microleakage. — Int J Implant Dent. — 2018; 4 (1): 11. PMID: 29629492
- Frost H.M. Bone «mass» and the «mechanostat»: a proposal. — Anat Rec. — 1987; 219 (1): 1—9. PMID: 3688455
- Kummer B.K.F. Biomechanics of bone: Mechanical properties, functional structure, functional adaptation. — In: Fung Y.C., Perrone N., Anliker M. (eds.) Biomechanics: Its Foundations and Objectives. — Englewood Cliffs: Prentice Hall, 1972. — Pp. 237—271.
- Figueras-Alvarez O., Cantó-Navés O., Real-Voltas F., Roig M. Protocol for the clinical assessment of passive fit for multiple implant-supported prostheses: A dental technique. — J Prosthet Dent. — 2020; S0022—3913 (20)30488—1. PMID: 33143900
- de Souza R.S., Suffredini I.B., Cortizo D.L., Larsson A., Nannmark U., Dib L.L. In vitro analysis of the implant-abutment interface connection and bacterial infiltration in two extraoral implant models. — Int J Oral Maxillofac Implants. — 2020; 35 (1): 63—9. PMID: 31923290
- Pammer D. Evaluation of postoperative dental implant primary stability using 3D finite element analysis. — Comput Methods Biomech Biomed Engin. — 2019; 22 (3): 280—287. PMID: 30676075
- Gvetadze R.Sh., Mikhas'kov S.V. Effectiveness of adjustment of bar constructions on implants by hydrogen and laser welding, metal soldering and electroerosive processing. — Stomatology. — 2011; 6: 50—1 (In Russ.).
- Goryainova K.E., Apresyan S.V., Lebedenko I.Yu., Voronov I.A. Comparative clinical evaluation of the prosthetic treatment quality of molars restored by chairside manufactured CAD/CAM crowns. — Stomatology. — 2019; 5: 72—7 (In Russ.).
- Iskenderov R.M., Gvetadze R.Sh., Butova V.G., Andreeva S.N., Timofeev D.E. General strategy for the development of dental laboratories with CAD/CAM systems. — Stomatology. — 2019; 2: 8—12 (In Russ.).
- Goo C.L., Tan K.B.C. Fabricating CAD/CAM implant-retained mandibular bar overdentures: A clinical and technical overview. — Case Rep Dent. — 2017; 2017: 9373818. PMID: 28396807
- Mangano F., Mangano C., Margiani B., Admakin O. Combining intraoral and face scans for the design and fabrication of computer-assisted design/computer-assisted manufacturing (CAD/CAM) polyether-ether-ketone (PEEK) implant-supported bars for maxillary overdentures. — Scanning. — 2019; 2019: 4274715. PMID: 31531155
- Oteiza-Galdón B., Martínez-González A., Escuder Á.-V. Analysis of fit on implants of chrome cobalt versus titanium frameworks made by cad / cam milling. — J Clin Exp Dent. — 2020; 12 (10): e951—7. PMID: 33154797
- Passaretti A., Petroni G., Miracolo G., Savoia V., Perpetuini A., Cicconetti A. Metal free, full arch, fixed prosthesis for edentulous mandible rehabilitation on four implants. — J Prosthodont Res. — 2018; 62 (2): 264—7. PMID: 29223315
- Srinivasan M., Schimmel M., Buser R., Maniewicz S., Herrmann F.R., Müller F. Mandibular two-implant overdentures with CAD-CAM milled bars with distal extensions or retentive anchors: A randomized controlled trial. — Clin Oral Implants Res. — 2020; 31 (12): 1207—22. PMID: 32965052
- Brånemark P.I., Hansson B.O., Adell R., Breine U., Lindström J., Hallén O., Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. — Scand J Plast Reconstr Surg Suppl. — 1977; 16: 1—132. PMID: 356184