DOI:
10.37988/1811-153X_2021_1_86Conditions of the jaw bone tissue at the stages of odontogenic desomorphine osteonecrosis treatment
Downloads
Abstract
Plural chronic odontogenic pockets of infection in drug addicts combined with application of fluorinated hand-crafted drugs effected in a growth of number of odontogenic osteonecrosis associated with drug intoxication. Desomorphine drug mixture includes derivatives of codeine and toxic substances. Various versions of surrogate drug synthesis presuppose different combinations of phosphorus, boric acid, alcohol solution of iodine and alcali. As a rule, necrotic lesions of jaws of drug addicts are diffuse ones never showing any tendency for demarcation at the first stages of disease. The aim of the study is to improve the provision of medical care to patients with osteonecrosis of the jaw.Materials and methods.
Within the period between 2008—2019 90 specific patients (19—55 years old, including 68% male parients and 32% female ones) got the surgical treatment at the maxilla-surgical unit. All abovementioned patients suffered from focal and diffuse osteonecrosis of the jaws, connected with the makeshift desomorphine application. Clinic case study shows, that bone tissue of maxilla and mandibula is a target organ, when speaking of the desomorphinic addiction. Exacerbation of chronic odontogenic pockets of infection and teeth extraction are the starting points of disease progression. That said, the integral part of phosphorus in the process of disease progression is supposed to be proven. As regards the etiology and pathogenesis, the disease may be referred to as the odontogenic toxic phosphoric osteonecrosis.
Results.
The present article dwells upon the question of jaw bone tissue structure alteration in the course of odontogenic osteonecrosis treatment provided to the patients, addicted to hand-crafted desomorphine, containing phosphorus. All the patients are subdivided into the following typical groups: 1) those suffering from tooth socket osteomyelitis after extraction of the tooth without tendency for demarcation, 2) those suffering from local osteonecrosis of dental segments, 3) those suffering from diffuse lesions of maxilla and mandibula, 4) those suffering from total lesion of facial skeleton and basis cranii, 5) convalescents with defects of jaws after the termination of necrosis inflammation. The present article describes the remodeling of bone after rejection and extraction of maxilla and mandibula sequestrum.
Conclusions.
The article presents a hypothesis, showing that preservation of the ossified periosteal layers, being formed around osteonecrosis area, is highly important for new formation of bone tissue after the admission of fluorinated hand-crafted drugs to the patient’s organism is stopped.
Key words:
osteonecrosis, desomorphine, drug addictionFor Citation
Introduction
The growth of cases of osteonecrosis of the jaws of various origin came to be one of the most burning problems of modern maxilla-facial and dental surgery all around the world [1—3]. As regards the development of the inflammatory process due to the chronic odontogenic pockets of infection as well as for the reason of the anatomic peculiarities of the maxilla-facial area, the above-mentioned area is the area at risk [4, 5]. The growth of the odontogenic inflammatory jaw diseases with necrotic predominance is connected with the rise of the new antiresorptive agents (i.e. bisphosphonates and Denosumab), as well as with the expansion of the crafted addictive substances, made up with the elemental phosphorus component [6—11].
Osteonecrosis of the jaws and other facial bones stands apart in the row of the odontogenic inflammatory diseases. The mentioned disease develops due to the injections of the unpurified reaction mixture, obtained in the process of hand-crafted desomorphine synthesis [12, 13]. Desomorphine (codeine derivative) is one of the opioid addictive substances, also known as “The crocodile” in Russia and other countries of the former USSR. “The crocodile”, being a hand-crafted substance, is a complex mixture of the organic materials, highly contaminated by the elemental phosphorus and its highly potent compounds [14—17].
Chronic odontogenic pockets of infection, being the component of pathogenesis of jaw osteomyelitis, accompanied by the drug intoxication, comes to be a starting point for the development of the diffuse necrotic process in the jaw bone tissue. The development of odontogenic proinflammatory process with the drug addicts is often an abnormal one. The longer is the term of drug addiction, the stronger are the infection symptoms [20, 21]. Experience made it possible to discover the following consistent pattern: as a rule, drug addict patients suffer from osteomyelitis (osteonecrosis) of the jaws, which have no tendency for demarcation [22, 23]. Extensive necrosis of the jaws and other facial bones makes the prognosis for the disease extremely unfavorable for such patients. It takes a radical surgery to save a life of such a patient [24—26].
The target of present study is to improve the provision of medical care to patients suffering from the osteonecrosis of the jaw:
- It is necessary to identify the typical groups of patients, suffering from the odontogenic osteonecrosis of the jaws.
- It is necessary to define the typical clinical and radiological symptoms on every stage of disease development.
- It is necessary to evaluate the dynamics of jaw bone tissue condition on every stage of the disease.
- It is necessary to work out the optimal tactics of the therapy of desomorphine osteonecrosis of the jaws.
Materials and methods
Within a period between 2008 and 2019 90 specific patients (19—55 years old, including 68% male patients and 32% female ones) underwent the surgical interference at the maxilla-surgical unit of the Alexander-Mariinsky regional hospital. All above-mentioned patients suffered from focal and diffuse osteonecrosis of the jaws due to the hand-craft desomorphine application. The study made it possible to define that 47% of the patients suffer from the focal lesions of the mandibular bone, 38% of the patients suffer from the focal lesions of the maxilla, and 15% of the patients suffer from the osteonecrosis of both maxilla and mandibular bones. Two more cases of the combined osteonecrosis of the maxilla, zygomatic bone and pterygoid process of sphenoid bone were observed as well. Diffuse lesion of the jaws amounted to 32% of all the cases, focal lesion — to 66%, and extensive facial bones lesions — to 2%. In the course of the study 2 patients, who underwent surgical interference, died (addictive substances overdose-induced death). 2 more patients died as a result of septic complications.
All the medical records of the above-mentioned ambulatory and hospital patients were evaluated in the course of a study, as well as CBCT, panoramic and multispiral computed tomography images of the jaws of all the patients in question.
Results
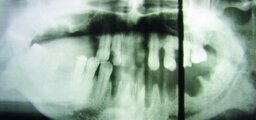
The disease onset in 99% of cases followed the teeth extraction, executed for the reason of the aggravation of a chronic periodontal disease. The case of development of the local osteonecrosis of the edentulous upper ridge came to be the only exception. The latter was connected with the damage to the oral mucosa due to the usage of the overdenture (Fig. 1).
It is possible to define 5 typical clinic and radiological groups of patients, suffering from various forms of the osteonecrosis of jaws and different complications.
The first group consists of the patients with the symptoms of tooth socket osteonecrosis, hospitalized within the period of 2—4 weeks following tooth extraction; patients, included in the first group, have a history of several unsuccessful attempts of ambulatory tooth socket inflammation therapy.
The second group consists of the following subgroups:
- the patients with the active clinical aspects of the focal osteonecrosis and local complications in the form of loosening of the healthy teeth, situated near the area of the primary defect;
- the patients suffering from the complications in the form of spontaneous perforation of the maxillary sinus or neuritis of the inferior alveolar nerve.
The third group consists of the patients suffering from:
- diffuse lesion of the jaw bone tissue;
- necrosis of mucosa above the damaged area;
- opening of the edentulous naked bone to the mouth cavity.
Diffuse infiltration of the facial soft tissues is typical for the patients of the third group (no abscesses or phlegmons were observed). Severe pain syndrome is also a typical effect. No sequestration were observed; CAT scans and X-ray images show the evidence of radiolucency without demarcation, although the tooth socket may stay visible.
The fourth group consists of the patients suffering from the overall lesion of maxilla and mandibula; osteonecrosis occupies facial skeleton and basis cranii. Spontaneous pathological fractures, development of the small plate-like sequesters and total loss of ordered jaw substance are considered to be the typical symptoms. CAT scans and X-ray images show the evidence of demarcation of the necrotizing areas. Multiple fistulas develop in the soft tissue (purulent discharge is quite poor). After drug intoxication is stopped, large sequesters gradually start to develop.
The fifth group consists of the convalescents after termination of the sequestration process. The typical complication of the disease is the bone remodeling, which mostly takes place in the area of mandibula. This complication manifests itself in the form of the new growth of the bone out of hypertrophied periosteum.
It is possible to define the typical clinical examples of the various groups of patients, suffering from odontogenic desomorphine osteonecrosis of the facial skeleton with the evidence of changes of the condition of the damaged bone tissue in the course of the disease progress.
Following symptoms are most typical for the first stages of disease:
- persistent defect after simple tooth extraction;
- spontaneous mucosal recession and opening of the naked bone into mouth cavity;
- long-term absence of the trend to the development and rejection of sequesters;
- absence of demarcation zone;
- aggravation of condition after osteonecrectomy, spreading of the lesion to the sound tissue areas.
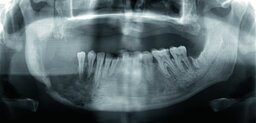
Tooth loss and mobility, sequestration of tooth sockets and upper ridge, of the fragments of maxillary body with the subsequent occurence of the penetration defect to the nasal cavity and maxillary sinus are the most typical findings (Fig. 2, 3).
As regards the perimaxillary and perimandibular soft tissue, the following occurrences are typically observed: diffuse infiltration around the lesion area and new growth of fistulas; extensive proinflammatory processes akin to the abscess or phlegmon are comparatively rare, and never exceed 5% of the whole number of the clinical events observed (Fig. 4).
The influence of the phosphorus and the role of the chronic odontogenic pockets of infection and teeth extraction during the period of pathogenesis of jaw osteonecrosis with the drug addicts, who regularly take makeshift desomorphine, is considered to be proven and quite obvious [27, 28]. All other cases present a typical clinical pattern: tooth extraction for the reason of the chronic periodontal disease recurrence is followed by the symptoms of the tooth socket inflammation and, further on, by the symptoms of the tooth socket osteomyelitis. Further on, the chronic focal osteonecrosis develops primarily, which tends to spread to the neighboring root segments (Fig. 5). The term of new growth of sequesters varies a lot and depends on continuation or termination of admission of the phosphatic mixtures to the body of the patient, as well as on the localization of the jaw osteonecrosis area [29].
Provided the patient is not treated properly or continues to take the addictive substances, the diffuse osteonecrosis of both maxilla and mandibula is inevitable. On the stage of further development osteonecrosis may spread to the zygomatic bone and basis cranii (Fig. 6).
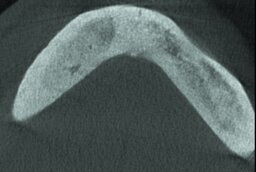
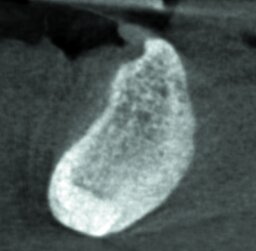
The study of the process of demarcation of the diffuse osteonecrosis enabled us to observe the remodeling and new growth of bone tissue as a result of ossification of the typical for the mentioned disease periosteal deposits, akin to the hyperplastic chronic osteomyelitis (Fig. 7). That enables us to assume that the preservation of the ossified periosteal deposits, growing around the mandibula osteonecrosis area, plays a key part in the restructuring and new growth of the bone tissue after abortion of the admission of the phosphatic mixtures to the body of the patient.
Following to the abortion of the necrotic process and rejection of sequesters or sequestrectomy, we observed the remodeling of the bone tissue, influenced by the masticatory muscles. The observation made it possible to detect several cases with the evidence of new growth of the bone tissue (up to 2 cm high and up to 10 cm in length), provided the bone continuity is preserved; in the event of the pathologic fractures immobilizing by means of the reconstructive plates is the necessary condition (Fig. 8). Articles of other authors confirm the phenomenon of the new growth of the bone tissue, described herein [30].
The above-mentioned remodeled bone is characterized by the reduced vascularity and high density, corresponding to the I type of the bone tissue according to Lekholm — Zarb (Fig. 9).
We have got the sufficient experience of the successful dental implantation, performed two and more years after abortion of the necrotic process in the bone tissue and termination of the drug addiction (Fig. 10). Our study also enabled us to observe clinical and radiological phenomenon of new growth of the bone tissue out of the ossified periosteum, preserved by some of patients after the near-total excision of the mandibula (Fig. 11).
Findings
The patients suffering from odontogenic desomorphine osteonecrosis may be divided into typical groups in accordance with the clinical and radiological symptoms, depending on the stage of the disease and according to the pathogenetic characteristics of the patient. The condition of the bone tissue on different stages of the phosphoric drug intoxication alters dynamically; the early disease detection and forehanded comprehensive therapy provide the necessary condition for the clinical outcome. The optimal tactics of therapy of the desomorphine osteonecrosis of the jaws consists of:
- the effective forehanded therapy of drug addiction;
- the abortion of admission of the phosphatic substances to the patient’s body;
- the reasonable surgery with the due consideration of the possibility of remodeling and even new growth of the bone tissue areas on the peripheral sites of the osteonecrosis zone after sequester rejection.
Conclusions
Hence, the condition of the bone tissue of the jaws of the patients suffering from the odontogenic desomorphine osteonecrosis of the jaws alters depending on the degree of the drug and phosphatic intoxication, as well as on the tactics of the therapy and the volume of surgery. The successful post-discharge adjustment of the patients, implying the application of the dentures fixed on the dental implants is considered to be a positive clinical outcome.
Figures


References
- Fleisher K.E., Kontio R., Otto S. Antiresorptive drug-related osteonecrosis of the jaw (ARONJ) — a guide to research. — Dubendorf (Switzerland): Foundation, 2017. — 64 p.
- Basin E.M., Medvedev Iu.A. Toxic phosphorous osteonecrosis of facial bones among drug addicts to desomorphine and pervitin. Part I. — Stomatology. — 2015; 2: 53—7 (In Russ.).
- Yarom N., Shapiro C.L., Peterson D.E. et al. Medication-related osteonecrosis of the jaw: MASCC/ISOO/ASCO clinical practice guideline. — J Clin Oncol. — 2019; 37 (25): 2270—90. PMID: 31329513
- Akopyan K.A. The state of the oral cavity of drug-dependent patients with osteonecrosis of the jaws, which takes the drug «crocodile» (desomorphine). — Journal of Dentistry and Maxillofacial Surgery. — 2012; 1: 16—9 (in Russ.).
- Babkova A.A. Complex radiological diagnosis of osteonecrosis in desomorphine dependence patients at the pre- and postoperative stages of treatment. — Russian Electronic Journal of Radiology. — 2016; 3: 21—9 (In Russ.).
- Hellstein J.W., Adler R.A., Edwards B., Jacobsen P.L., Kalmar J.R., Koka S., Migliorati C.A., Ristic H., American Dental Association Council on Scientific Affairs Expert Panel on Antiresorptive Agents. Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs. — J Am Dent Assoc. — 2011; 142 (11): 1243—51. PMID: 22041409
- Egloff-Juras C., Gallois A., Salleron J., Massard V., Dolivet G., Guillet J., Phulpin B. Denosumab-related osteonecrosis of the jaw: A retrospective study. — J Oral Pathol Med. — 2018; 47 (1): 66—70. PMID: 28977694
- Hamadeh I.S., Ngwa B.A., Gong Y. Drug induced osteonecrosis of the jaw. — Cancer Treat Rev. — 2015; 41 (5): 455—64. PMID: 25913713
- Booth R.E. “Krokodil” and other home-produced drugs for injection: a perspective from Ukraine. — Int J Drug Policy. — 2013; 24 (4): 277—8. PMID: 23764188
- Timofeev A.A. Clinical course and surgical treatment of purulent-inflammatory diseases of the jaw in people who use drugs. — Modern dentistry. — 2015; 1: 62—70 (In Russ.).
- King R., Tanna N., Patel V. Medication-related osteonecrosis of the jaw unrelated to bisphosphonates and denosumab-a review. — Oral Surg Oral Med Oral Pathol Oral Radiol. — 2019; 127 (4): 289—99. PMID: 30713092
- Basin E.M. Toxic phosphorous osteonecrosis of the facial skeleton: dissertation abstract. — Moscow: Sechenov University, 2017. — 48 (In Russ.).
- Sergent J.-F., Bader G., Hamon J., Peigne L., Lejeune S. Krokodil (desomorphine)-induced osteonecrosis of the maxilla: a case report and literature review. — Journal of Oral Medicine and Oral Surgery. — 2019; 25: 26. DOI: 10.1051/mbcb/2019011
- Gahr M., Freudenmann R.W., Hiemke C., Gunst I.M., Connemann B.J., Schönfeldt-Lecuona C. Desomorphine goes “crocodile”. — J Addict Dis. — 2012; 31 (4): 407—12. PMID: 23244560
- Skowronek R., Celiński R., Chowaniec C. “Crocodile” — new dangerous designer drug of abuse from the East. — Clin Toxicol (Phila). — 2012; 50 (4): 269. PMID: 22385107
- Hout M.C.V. Kitchen chemistry: A scoping review of the diversionary use of pharmaceuticals for non-medicinal use and home production of drug solutions. — Drug Test Anal. — 2014; 6 (7—8): 778—87. PMID: 24619569
- Kempen E.E.J., Brand H.S. Effects of krokodil (desomorphine) use on oral health — a systematic review. — Br Dent J. — 2019; 227 (9): 806—12. PMID: 31705099
- Shevchenko L.V., Lozhkin D.A. Features of treatment of patients with chronic osteomyelitis of the jaw against the background of taking narcotic drugs. — Proceedings of the IX conference “Dentistry of the Slavic States”. — Belgorod, 2016. — Pp. 482—485 (In Russ.).
- Saberov R.Z., Drobyshev A.U. Characteristics of the surgical service of osteonecrosis jaws on background of the drug dependence. — International Dental Review. — 2013; 3: 26—33 (In Russ.).
- Malanchuk V. A., Brodetsky I.S. Complex treatment of patients with osteomyelitis of the jaws against the background of drug addiction. — Vestnik of Vitebsk State Medical University. — 2014; 2: 115—23 (In Russ.).
- Ruzin G.P., Tkachenko O.V. Clinical manifestations of toxic osteomyelitis depending on the prescription of drug use. — Ukrainian Dental Almanac. — 2015; 1: 47—52 (In Russ.).
- Ruzin G.P., Tkachenko O.V., Myroshnychenko M.S., Pliten O.N., Myroshnychenko A.A. Chronic toxic osteomyelitis in patients that taken the drug pervitin. — Tavricheskiy Mediko-Biologicheskiy Vestnik. — 2013; 1—2; 167—9 (In Russ.).
- Medvedev Yu.A., Basin E.M., Serova N.S., Korshunova A.V., Babkova A.A., Kureshova D.N. Total jaw osteonecrosis among drug addicts. — Russian Journal of Dentistry. — 2016; 4 (20): 183—9 (In Russ.).
- Landyshev Y.S., Goborov N.D., Tsukanova G.D. Infectious complications in chronic desomorphine addiction. — Amur Medical Journal. — 2017; 1(17): 76—81 (In Russ.).
- Nesterov O.V., Ilina R.U., Urakova E.V. Tactics and treatment of primary chronic deomorphine osteomyelitis. — Proceedings of th “Biocompatible materials and new technologies in dentistry” conference. — Kazan, 2014. — Pp. 231—235 (In Russ.).
- Medvedev Iu.A., Basin E.M., Korshunova A.V. Surgical treatment of patients with drug abuse and mandible necrosis. — Stomatology. — 2014; 93 (5): 40—2 (In Russ.).
- Basin E.M., Medvedev Iu.A. toxic phosphorous osteonecrosis of facial bones among drug addicts to desomorphine and pervitin. Part II. — Stomatology. — 2015; 3: 67—9 (In Russ.).
- Poghosyan Y.M., Hakobyan K.A., Poghosyan A.Y., Avetisyan E.K. Surgical treatment of jaw osteonecrosis in “Krokodil“ drug addicted patients. — J Craniomaxillofac Surg. — 2014; 42 (8): 1639—43. PMID: 24969764
- Antakov G.I., Shtraube G.I., Boev I.A. Sequestration periods for toxic osteonecrosis of the lower jaw, depending on the extent of bone damage. — The Dental Institute. — 2019; 1 (82): 68—71 (In Russ.).
- Hakobyan K., Poghosyan Y. Spontaneous bone formation after mandible segmental resection in “krokodil” drug-related jaw osteonecrosis patient: case report. — Oral Maxillofac Surg. — 2017; 21 (2): 267—70. PMID: 28251363