DOI:
10.37988/1811-153X_2021_1_114Algorithm for comprehensive diagnosis and treatment of patients with gnathic form of malocclusion class II (clinical case)
Downloads
Abstract
The aim of the study was to improve the diagnosis and treatment of patients with gnatic forms of malocclusions. The article has a clinical case of comprehensive treatment of a 18-year-old female patient with gnathic form of malocclusion class II. We carried out comprehensive diagnosis of the patient’s dentition: clinical examination; photometry; anthropometry of the dentition on plaster models; X-ray; kinesiography of the lower jaw; electromyography of muscles of maxillofacial region. Then, a treatment plan for the patient was drawn up, consisting of the orthodontic and surgical stages. The surgical stage included carrying out an orthognathic two-jaw operation using a surgical template (splint) made according to our method. After the comprehensive treatment, an optimal aesthetic and functional result was achieved, which was confirmed by comprehensive diagnostics. The proposed method of treatment using a splint made it possible to shorten the surgery time and reduce the risk of possible complications and was successfully applied in the comprehensive treatment of 2 patients with gnathic form of malocclusion class II.Key words:
malocclusion class II, gnathic form, orthognathic surgery, splintFor Citation
Introduction
According to Russian and foreign authors, maxillofacial anomalies are found in 33—70% of the examined patients [1—5]. During the orthodontic treatment of patients with gnathic (skeletal) form of malocclusions it is not always possible to achieve optimal aesthetic and functional results, because this pathology often requires surgical correction of the size and position of the jaws [6—12]. In such cases comprehensive approach is required, including the orthodontic and surgical stages of treatment. Modern orthognathic surgery is provided with tools that make it possible to predict the postoperative outcome accurately [13—18]. Comprehensive diagnostics is necessary to select the optimal treatment method and minimize possible complications [19—22].
The aim of the study is to improve the diagnosis and treatment of patients with gnathic forms of malocclusions.
Materials and methods
The diagnostics and the orthodontic stage of treatment were carried out at the clinical base of the department of postgraduate dentistry, at the department of therapeutic dentistry of SSMU and in Postnikov multidisciplinary clinic. We conducted clinical examination, photography, anthropometry of the dentition on plaster models. X-ray research methods were used: orthopantomography (OPTG), teleradiography (TRG), cone-beam computed tomography (CBCT) of the facial region of the skull and temporomandibular joint (TMJ) on the right and left in the position of the closed and open mouth. The functional research methods were kinesiography (CG) of the lower jaw and electromyography (EMG) of muscles of the maxillofacial region [23].
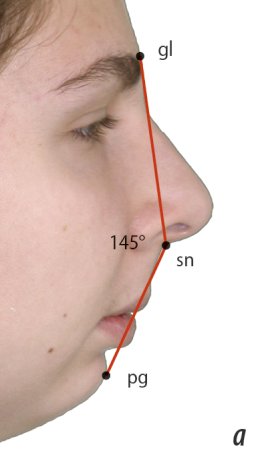
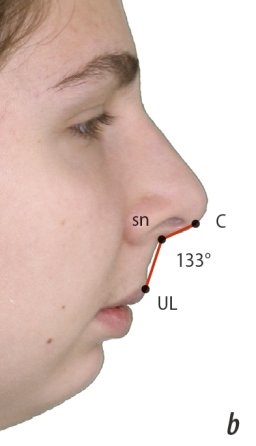
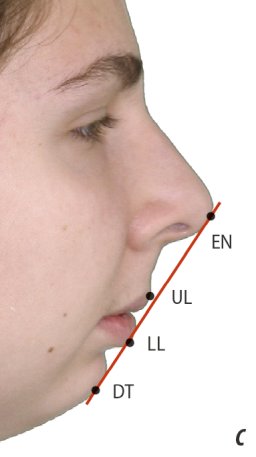
We made photography of full face with and without a smile, in profile, and 3/4 of a turn. In profile photographs, the angle of facial convexity was measured (∠gl /sn /pg) and the profile type was determined according to Arnett and Bergman, the nasolabial angle (∠c-sn—UL) was measured, labial steps were found according to Corkhouse, and the position of the lips relative to the Ricketts aesthetic line was determined (E-lines). Izar's facial index was used to analyze the head from the front.
Anthropometry included measuring the mesiodistal size of the teeth, length of the anterior segment of the dentition, width of the dentition in the canines segment, premolars and molars, and the width and length of the apical bases. The Tone and Bolton indices were calculated, the sizes of the dentition were determined using the methods of Pon, Korkhouse, Slabkovskaya, House-Snagina (LS Persin, 2016).
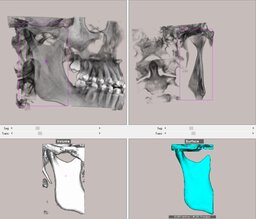
Radiography was performed on a Planmeca ProMax 3D Classic (Finland) in the “M” imaging mode, in which the program automatically sets the voltage of 66 kV and the current strength of 8 mA in the X-ray tube. The TRG analysis was carried out using the Dolphin Imaging (USA) in the Ceph Tracing module and included finding the SNA and SNB, ANB angles, the Wits number, the length of the ANS—PNS and Go—Pg segments, as well as the U1—SN, L1—MP angles and the interincisal angle [24—27]. The analysis of CBCT of the TMJ was carried out according to the method of N.A. Rabukhina [28].
The study of function of the dentition was carried out using BioKET / Biotronic equipment (Italy), which includes a kinesiograph and a 16-channel electromyograph. The CG included the following tests: mouth opening; myocentric; swallowing; protrusion; laterotrusion. During EMG, the following tests were performed: state of relative physiological rest; primary contact of antagonist teeth; a state of relative physiological rest while standing; repeated occlusal contacts; swallowing; maximum compression of the jaws; functional test under load (with rollers) [29]. The existing anomalies were classified according to the classification of Khoroshilkina F.Ya., which distinguishes dentoalveolar, gnathic and combined forms of maxillofacial anomalies.
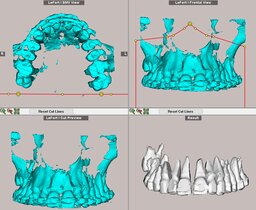
During orthognathic surgery, a surgical template (splint) was used to match the jaws to the position of a constructive bite, which was digitally manufactured [30, 31]. Manufacturing steps:
- Taking optical impressions and making digital models of the jaws before surgery.
- Conducting CBCT of the patient's facial section of skull before surgery.
- CBCT of the patient's facial section of skull is combined with an optical model of the patient's dentition in the Dolphin Imaging (3D module) before surgery.
- Anthropometric and cephalometric analysis of jaw CBCT in Dolphin Imaging before surgery.
- Planning a virtual gnathic surgery in Dolphin Imaging under the supervision of an orthodontist and maxillofacial surgeon.
- Three-dimensional modeling of the surgical template and its manufacture in the laboratory.
For the proposed method of manufacturing a surgical template we received a patent of the Russian Federation No. 195882.
Clinical case
Patient G., 18 years old, complained of a cosmetic defect of face (“bird's face”), incorrect position of teeth. She was recommended to consult an orthodontist by a dentist. Previously, she did not undergo orthodontic treatment.
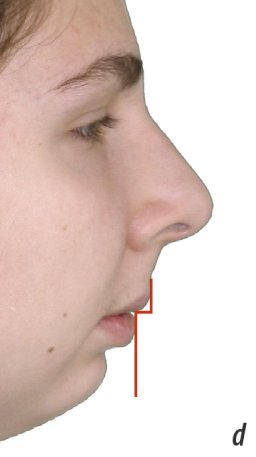
An external examination of the face profile revealed a defection of the aesthetics of the face profile — retrognathia of the lower jaw. Chin is slightly displaced to the right (Fig. 1).
Oral examination:
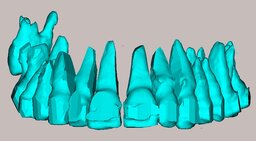
- Sagittal direction — closing of the first molars according to class II by Engle on both sides, closing of the canines — II class on the right, I class on the left; sagittal fissure — 9.4 mm, sagittal incisal disocclusion.
- Vertical direction — vertical gap of 3.5 mm within 4 anterior teeth, there is no vertical gap in the lateral segments.
- Transversal direction — displacement of the central line on the upper jaw to the right by 4 mm, cross occlusion on the right (Fig. 2).
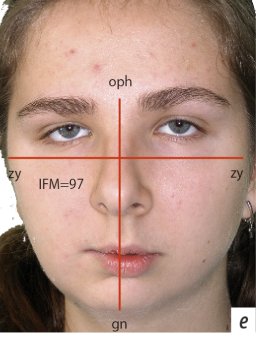
According to the analysis of photographs of the patient's face in frontal view and profile, it was revealed: the value of the angle of the convexity of face is 145° (malocclusion class II and convex profile), the nasolabial angle is 133° (above normal), the protrusion of the lower lip relative to the aesthetic line of Ricketts, the labial step according to Corkhouse is pronounced negative, the Izar index is 97 (medium face shape; Fig. 3).
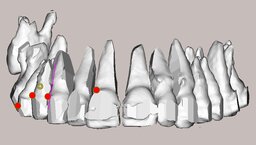
Anthropometry of the dentition on plaster models showed the following results: Tone index is equal to 1.42; the Bolton index was not taken into account due to the absence of teeth 1.4 and 2.4; the width in the canines segment of the upper jaw is less than the individual norm by 2 mm, the lower jaw is normal, in the premolars segment of the upper jaw it is less by 6 mm, the lower jaw is less by 4 mm, the molars segment of the upper jaw it is less by 8 mm, the lower jaw is less by 6 mm; the length of the anterior segment of the dentition of the upper jaw is more by 3 mm, of the lower jaw — less by 5 mm; the length of the apical base of the upper jaw is more by 7 mm, the lower one is less by 9 mm; the width of the apical base of the upper jaw is less by 8 mm, the lower one is less by 6 mm.
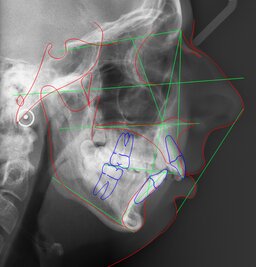
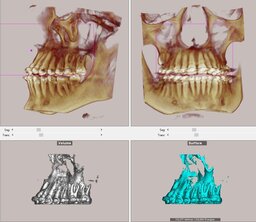
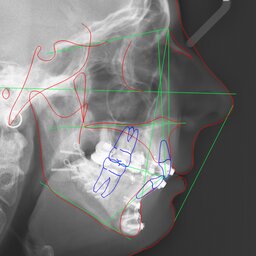
According to OPTG, the patient has 28 teeth. Teeth 1.4, 1.8, 2.4 and 3.8 are missing (Fig. 4). Analysis of the patient's TRG showed that the SNA angle is slightly reduced — 78.3°, the SNB angle is greatly reduced — 68.5°, the size of the upper jaw is within the individual norm, the lower jaw is reduced by 21.4 mm, the ANB angle is 9.8°, the Wits appraisal is 12.8 mm, the position of the central incisors of the upper and lower jaws is normal, the interincisal angle is less than normal (Fig. 5). This data make it possible to diagnose a gnathic form of malocclusion class II caused by microgenia of the lower jaw. The S—Go/Na—Me face height ratio is 62.6, due to a decrease in the S—Go back face height. The height of the middle third of the face N—ANS is reduced, the height of the lower third of the face ANS—Gn is within normal limits.
Analysis of CBCT of the temporomandibular joint according to the method of N.A. Rabukhina showed that the width of the joint space of the right temporomandibular joint in the anterior section is 2.60 mm, in the middle section — 2.24 mm, in the posterior — 2.28 mm, in the left temporomandibular joint — 2.06, 1.97 and 1.90 mm respectively. A change in the shape of head of the lower jaw on the right was found.
According to the results of the kinesiography of the lower jaw, it was revealed: non-uniform movement of the lower jaw when opening and closing the mouth; deflection of the lower jaw to the right by 3.40 mm; decrease in the amplitude of opening the mouth; a decrease in the lowering speed of the lower jaw to 69 mm/s (the norm is 171—197 mm/s); a decrease in the speed of raising the lower jaw to 60 mm/s (the norm is 264—295 mm/s); decrease in the length of the diagonal — 21.14 mm (norm 50.77—51 mm); an increase in the value of the working angle — 64.43° (norm 38.86—40°). There is a discrepancy between the graphs of “myocentric” and “swallowing”, a change in the function of swallowing, while the graph of “myocentric” in the frontal plane is shifted to the left, and the amplitude of movements is reduced. During the “protrusion” and “laterotrusion” tests contact instability was revealed, the range of motion was reduced, and the "protrusion" graph in the frontal plane was shifted to the right. Found functional changes in the TMJ.
According to the EMG results asymmetric muscle work was revealed. In the test “repeated occlusive contacts” the biopotential of the left m. temporalis and m. masseter is higher than on the right. In the tests “swallowing”, “maximum compression of the jaws”, “functional test under load” we revealed cross asymmetry — right m. temporalis is tense more than the left, the left m. masseter is more tense than the right. In all samples, except for the functional test under load, the biopotential mm. temporalis is higher than that of mm. masseter.
| Test | Muscle | Average amplitude (μV) | |
| Right | Left | ||
| Relative physiological rest | M. temporalis | 5 | 4 |
| M. masseter | 3 | 3 | |
| Mm. suprahyoidei | 3 | 4 | |
| M. sternocleidomastoideus | 7 | 9 | |
| Initial contact of the antagonist teeth of the upper and lower jaws | M. temporalis | 12 | 12 |
| M. masseter | 3 | 4 | |
| Mm. suprahyoidei | 3 | 4 | |
| M. sternocleidomastoideus | 7 | 9 | |
| Relative physiological rest while standing | M. temporalis | 5 | 6 |
| M. masseter | 4 | 3 | |
| Mm. suprahyoidei | 5 | 5 | |
| M. sternocleidomastoideus | 7 | 10 | |
| Repeated occlusal contacts | M. temporalis | 24 | 31 |
| M. masseter | 9 | 42 | |
| Mm. suprahyoidei | 5 | 5 | |
| M. sternocleidomastoideus | 7 | 9 | |
| Swallowing | M. temporalis | 33 | 18 |
| M. masseter | 8 | 14 | |
| Mm. suprahyoidei | 59 | 49 | |
| M. sternocleidomastoideus | 10 | 10 | |
| Maximum compression of the jaws | M. temporalis | 85 | 78 |
| M. masseter | 23 | 60 | |
| Mm. suprahyoidei | 6 | 6 | |
| M. sternocleidomastoideus | 7 | 9 | |
| Functional test under load | M. temporalis | 116 | 107 |
| M. masseter | 138 | 150 | |
| Mm. suprahyoidei | 21 | 19 | |
| M. sternocleidomastoideus | 9 | 10 | |
According to the diagnostics, a plan was drawn up, and the following stages of treatment were performed:
- Consultation of the patient with an orthodontist and maxillofacial surgeon. Obtaining impressions and plaster models of the dentition, anthropometry of the dentition on plaster models, drawing up a plan for comprehensive treatment, planning upcoming operations and their sequence.
- Pre-surgical orthodontic stage, which consisted of dentoalveolar decompensation of the anomaly using the Damon Q bracket system (6 months). At this stage, the shapes of the dentition were aligned and normalized to achieve their congruence.
- Cephalometric analysis of the facial segment of skull (Fig. 6). It was decided to carry out a two-jaw operation: first on the lower jaw, and after 1.5—2.5 months of rehabilitation — on the upper jaw.
- The data about the planned movement of the jaws were transferred to the articulator with the plaster cast of the patient's jaws. The criterion for the patient's readiness for the surgical stage was a comparison of the jaw models in a constructive bite in an articulator according to Angle class I based on the obtained parameters of movement, as well as the correct position of the incisors of the upper and lower jaw according to three-dimensional planning data.
- Making a splint for correct positioning of the jaw during surgery. A surgical template (splint) was made in the dental laboratory from plastic and holes were drilled for the further placement of mini-screws in them at pre-designated points.
- Fitting the template in the oral cavity before the operation to check the contacts. Then the patient was referred to the surgical department for an osteotomy of the mandible.
- First surgery — bilateral sagittal retromolar osteotomy of the mandible according to Dal Pont. The fragments of jaw are fixed with titanium mini-plates, which ensure the stability of the position of the jaw segments. The jaw was immobilized for 1 month with screws for intermaxillary fixation.
- During orthodontic treatment, 1.5 months after the first operation, measures were taken to achieve tight fissure-tubercular contacts using intermaxillary elastics.
- The second surgery — osteotomy of the upper jaw of type I according to LeFor with cutting off the septum of the nose and vomer. The resected fragment was positioned in the previously predicted position in accordance with the occlusal plane and its position was fixed with titanium mini-plates. The wounds were sutured tightly.
- 5 months after the second operation — orthodontic treatment for 2 months to achieve tight fissure-tubercular contacts using intermaxillary elastics.
- The retention period (3—5 years). After removing the orthodontic appliances (braces) patient continued wearing the intermaxillary elastics for 6 months to achieve stable retention (Fig. 7). The treatment was completed with the making of a fixed retention device for the lower jaw and a removable one for the upper jaw.
Results
After the treatment an optimal functional and aesthetic result was achieved (Fig. 8, 9). Analysis of photographs of patient's face in frontal view and profile showed: an increase in the value of the angle of facial convexity from 145° to 154°, which indicates a shift of this indicator towards physiological occlusion and a straight profile (165—175°); a decrease in the value of the nasolabial angle from 133° to 125°, which took this indicator closer to the norm (100—110°); the position of lips relative to the aesthetic line of Ricketts began to correspond to a harmoniously developed face; decrease in the severity of the labial step according to Korkhouse; the value of the Izar index remained unchanged. No relapses occurred during the retention period. Comprehensive diagnostics based on the results of treatment showed an improvement in the parameters of the anatomical and functional state of the maxillofacial system. Analysis of TRG showed: an increase in the value of the SNB angle from 68.5° to 69.2° and its approximation to the norm (80±2°); a decrease in the value of the ANB angle from 9.8° to 9.2° (norm 2—4°) and Wits-number from 12.8 mm to 4.6 mm (norm —1 mm), which indicates the normalization of the intermaxillary ratio; an increase in the value of the inter-incisal angle from 116° to 125.7°, which became within the normal range (130±5°; Fig. 10).
Conclusion
The proposed method of treatment using a splint made it possible to shorten the surgery time and reduce a risk of possible complications.
During the comprehensive (orthodontic and surgical) treatment of patient with a gnathic form of malocclusion class II, an optimal aesthetic and functional result was achieved.
When studying the methods of treatment of gnathic forms of bite using of a classic splint and a splint with holes for a microimplant, the advantages of our method were revealed.
The surgical template (splint), modeled in the surgical module of the Dolphin Imaging, has been successfully used in the comprehensive treatment of 2 patients with a gnathic form of malocclusion class II; the proposed method can also be used in patients with a gnathic form of malocclusion class III.
Figures
References
- Arsenina O.I., Popova A.V., Popova N.V. Treatment of patients with dentoalveolar anomalies and functional disorders using elastocorrector. — Moscow: Central Research Institute for Dentistry and Maxillofacial Surgery, 2016. — P. 7—17 (In Russ.).
- Khoroshilkina F.Ya. Orthodontics. Defects of teeth, dentition, malocclusion, morphological and functional disorders in the maxillofacial region and their complex treatment. — Moscow: Medical Information Agency, 2006. — P. 26—34 (In Russ.).
- Alhammadi M.S., Halboub E., Fayed M.S., Labib A., El-Saaidi C. Global distribution of malocclusion traits: A systematic review. — Dental Press J Orthod. — 2018; 23 (6): 40.e1—40.e10. PMID: 30672991
- Zou J., Meng M., Law C.S., Rao Y., Zhou X. Common dental diseases in children and malocclusion. — Int J Oral Sci. — 2018; 10 (1): 7. PMID: 29540669
- Stepanov G.V., Dikova A.A., Ulyanova L.G., Postnikov M.A., Chigarina S.E., Khamadeeva A.M. Treatment of patients with the malposition of individual teeth in patients with sagittal occlusion anomalies. — International Journal of Psychosocial Rehabilitation. — 2020; 5 (24): 5019—37. eLIBRARY ID: 43282475
- Fowler P., King T., Lee M., Erasmus J. Retrospective study of eligibility for orthognathic surgery using the Index of Orthognathic Functional Treatment Need (IOFTN). — Br J Oral Maxillofac Surg. — 2018; 56 (5): 416—20. PMID: 29678373
- Geramy A., Sheikhzadeh S., Jalali Y.F., Nazarifar A.M. Anthropometric facial changes after orthognathic surgery and their relation with oral health related quality of Life. — J Craniofac Surg. — 2019; 30 (4): 1118—20. PMID: 31166256
- Pace M., Cioffi I., D'antò V., Valletta A., Valletta R., Amato M. Facial attractiveness of skeletal class I and class II malocclusion as perceived by laypeople, patients and clinicians. — Minerva Stomatol. — 2018; 67 (3): 77—85. PMID: 29308854
- Eslami S., Faber J., Fateh A., Sheikholaemmeh F., Grassia V., Jamilian A. Treatment decision in adult patients with class III malocclusion: surgery versus orthodontics. — Prog Orthod. — 2018; 19 (1): 28. PMID: 30069814
- Hwang B.-Y., Choi B.-J., Lee B.-S., Kwon Y.-D., Lee J.-W., Jung J., Ohe J.-Y. Comparison between anterior segmental osteotomy versus conventional orthodontic treatment in root resorption: a radiographic study using cone-beam computed tomography. — Maxillofac Plast Reconstr Surg. — 2017; 39 (1): 34. PMID: 29204418
- Tachiki C., Yamamoto M., Takaki T., Nishii Y. Surgical orthodontic treatment in case of severe high angle skeletal class II malocclusion and mandibular retrusion. — Bull Tokyo Dent Coll. — 2020; 61 (4): 243—53. PMID: 33177274
- Starch-Jensen T., Blæhr T.L. Transverse expansion and stability after segmental Le Fort I osteotomy versus surgically assisted rapid maxillary expansion: a systematic review. — J Oral Maxillofac Res. — 2016; 7 (4): e1. PMID: 28154745
- Naran S., Steinbacher D.M., Taylor J.A. Current concepts in orthognathic surgery. — Plast Reconstr Surg. — 2018; 141 (6): 925e—936e. PMID: 29794714
- Iwamoto M., Watanabe M., Yamamoto M., Narita M., Kamio T., Takaki T., Shibahara T., Katakura A. Prognostic factors for maxillary sinus mucosal thickening following Le Fort I osteotomy: a retrospective analysis. — Maxillofac Plast Reconstr Surg. — 2019; 41 (1): 12. PMID: 30915318
- Ann H.-R., Jung Y.-S., Lee K.-J., Baik H.-S. Evaluation of stability after pre-orthodontic orthognathic surgery using cone-beam computed tomography: A comparison with conventional treatment. — Korean J Orthod. — 2016; 46 (5): 301—9. PMID: 27668193
- Kim H., Cha K.-S. Evaluation of the stability of maxillary expansion using cone-beam computed tomography after segmental Le Fort I osteotomy in adult patients with skeletal Class III malocclusion. — Korean J Orthod. — 2018; 48 (1): 63—70. PMID: 29423378
- Lin L., Fan B., Yu Z., Xu L., Yuan J., Wu J., Wei M. Application of computer-assisted navigation in mandibular angle osteotomy. — J Int Med Res. — 2019; 47 (7): 3160—70. PMID: 31204540
- Cappellozza J.A.Z., Guedes F.P., Filho H.N., Filho L.C., de Almeida Cardoso M. Orthodontic decompensation in skeletal class III malocclusion: redefining the amount of movement assessed by cone-beam computed tomography. — Dental Press J Orthod. — 2015; 20 (5): 28—34. PMID: 26560818
- Dybov A.M., Denisova E.A., Ospanova G.B., Mamedov A.A. Diagnosis and planning of complex aesthetic-functional rehabilitation of patients with asymmetrical dentoalveolar anomalies. — Clinical Dentistry (Russia). — 2019; 1 (89): 76—81 (In Russ.).
- Arkhipov A.V., Loginova E.A., Arkhipov V.D. Modern methods of diagnosis in orthodontics. — Science and innovation in medicine. — 2016; 2 (2): 10—3 (In Russ.).
- Postnikov M.A., Nesterov A.M., Trunin D.A., Sadykov M.I., Gabdrafikov R.R., Sagirov M.R. Possibilities of diagnostics and complex treatment of patients with TMJ disfunctions. — Clinical Dentistry (Russia). — 2020; 1 (93): 60—3 (In Russ.).
- Lo Giudice A., Quinzi V., Ronsivalle V., Farronato M., Nicotra C., Indelicato F., Isola G. Evaluation of imaging software accuracy for 3-dimensional analysis of the mandibular condyle. A comparative study using a surface-to-surface matching technique. — Int J Environ Res Public Health. — 2020; 17 (13): 4789. PMID: 32635238
- Giannini L., Maspero C., Galbiati G., Kairyte L., Zanoni F., Farronato G. Orthodontic-surgical treatment: electromyographic and kinesiographic evaluation in follow up period. Experimental study. — Stomatologija. — 2017; 19 (2): 35—43. PMID: 29243682
- Semenov M.G., Kudryavtseva O.A., Stetsenko A.G., Filippova A.V. Modern methods of craniometrical analysis in reconstructive surgery planning on the facial skull in the growing organism. — Institute of Dentistry. — 2015; 1 (66): 48—51 (In Russ.).
- Peterman R.J., Jiang S., Johe R., Mukherjee P.M. Accuracy of Dolphin visual treatment objective (VTO) prediction software on class III patients treated with maxillary advancement and mandibular setback. — Prog Orthod. — 2016; 17(1):19. PMID: 27312722
- Plaza S.P., Reimpell A., Silva J., Montoya D. Relationship between skeletal Class II and Class III malocclusions with vertical skeletal pattern. — Dental Press J Orthod. — 2019; 24(4):63—72. PMID: 31508708
- Karabekmez F.E., Kleinheinz J., Jung S. Dimensions of velopharyngeal space following maxillary advancement with Le Fort I osteotomy compared to Zisser segmental osteotomy: A cephalometric study. — Biomed Res Int. — 2015; 2015: 389605. PMID: 26273615
- Postnikov M.A., Trunin D.A., Pankratova N.V., Slesarev O.V. Clinical and X-ray methods of diagnostic in dentistry: students book — Samara: Publishing and Printing Complex» Pravo «, 2021. — Pp. 92—94 (In Russ.).
- Dubova L.V., Melnik A.S., Stupnikov A.A., Savelyev V.V. Comparative evaluation of data kineseography and electromyography at patients without signs of TMJ disorders and with. — Endodontics today. — 2016; 2: 11—15 (In Russ.).
- Postnikov M.A., Trunin D.A., Nesterov A.M., Gabdrafikov R.R., Sadykov M.I., Potapov V.P., Pankratova N.V. Use of occlusal digital splint for treating the patients with temporomandibular joint dysfunction and planning orthopedic treatment. — Russian Open Medical Journal. — 2020; 9(2): 7—14. eLIBRARY ID: 43307527
- Shirota T., Shiogama S., Asama Y., Tanaka M., Kurihara Y., Ogura H., Kamatani T. CAD/CAM splint and surgical navigation allows accurate maxillary segment positioning in Le Fort I osteotomy. — Heliyon. — 2019; 5 (7): e02123. PMID: 31372564