DOI:
10.37988/1811-153X_2021_1_80Autologous dental transplantation in a patient congenital cleft of the lip, alveolar process and palate
Downloads
Abstract
This article examines bone grafting of the alveolar process with simultaneous autologous tooth transplantation in patients congenital cleft of the lip, alveolar process and palate.Materials and methods.
At the Department of maxillofacial surgery and hospital surgical Dentistry from October 2016 to present, 26 patients between the ages of 9 to 12 years with congenital cleft of the upper lip, alveolar process and palate were clinically examined and treated. Patients underwent bone grafting of the alveolar process of the upper jaw with simultaneous autologous tooth transplantation and the use of miniplates. During the year monitoring with x-ray control was performed to assess the degree of resorption of bone regenerate and the apical part of the roots of autotransplanted teeth.
Results.
The proposed method of bone grafting of the alveolar process with simultaneous autotransplantation allowed to stabilize the fragments of the upper jaw, restore the volume of the alveolar process in the cleft area, and to restore the dentition.
Conclusion.
The resulting clinical results and postoperative assessment of the bone structure after bone grafting of the alveolar process with simultaneous autologous tooth transplantation and fixation of fragments of the upper jaw using mini-plates provide a predictable result of restoring the volume of the alveolar process and restoring the dentition.
Key words:
dystopia, retention, adentia, autologous dental transplantation, augmentation, bone grafting, bone substitutes, cleft, alveolar processFor Citation
Introduction
One of the most common malformations of the maxillofacial region is a congenital cleft of the upper lip, alveolar process and palate (UCLP), which is formed during histogenesis under the influence of various teratogenic factors [1, 2]. Patients with this defect need long-term multi-stage rehabilitation [3, 4]. Bone grafting of the alveolar process of the upper jaw [5] aimed not only at restoring anatomical integrity, but also at creating a volume of bone tissue for subsequent dental implantation, in order to restore chewing function, diction and aesthetics [6]. Therefore, in the complex rehabilitation of such patients, it is mandatory to include surgical and orthodontic measures [7—9].
There are patients with congenital cleft of the upper lip, alveolar process and palate, a violation of dentition, dystopia and retention or adentia of the rudiments of permanent teeth, underdevelopment of the upper and lower jaw, which affects not only the appearance of the patient, but also leads to such functional disorders as difficulty chewing food, impaired respiratory function [10].
In addition, patients have an oronasal anastomosis, which leads to food entering the nasal cavity, causing the development of a chronic inflammatory process, as well as the appearance of fear of eating in public places [11].
According to many authors, the optimal age for bone grafting of the alveolar process of the upper jaw in congenital cleft is 8—11 years, which corresponds to the time of eruption of the permanent canine germ. Since the subsequent eruption of the permanent canine germ occurs in the area of bone regenerate, which contributes not only to its stabilization in the correct physiological position [12, 13], but also to the subsequent preservation of the volume of bone regenerate, due to the subsequent functional load on it. If it is impossible or untimely to carry out this stage of rehabilitation, the canine eruption occurs in the cleft area, with the absence of bone tissue adjacent to the root part of the tooth and the subsequent loss of a permanent tooth. If given patients with congenital cleft of the upper lip, alveolar process and palate often have concomitant retention or adentia of the lateral incisor on the side of the cleft, which exacerbates violations of the dentition and deterioration of the aesthetics of the smile.
Currently, the restoration of the dentition in patients with congenital cleft lip, alveolar process and palate carried out in several ways, such: partial removable prosthetics, non-removable prosthetics with metal-ceramic structures, as well as dental implantation. All of the above methods have a number of disadvantages and, with the exception of a removable prosthesis, not used during skeletal growth.
Thus, in patients with UCLP, if the recommended age range observed, from bone grafting of the alveolar process to the installation of a dental implant, the time interval is about 7—9 years, such a long absence of functional load on the bone regenerate contributes to significant resorption, which further requires repeated bone grafting.
One of the ways to restore the dentition in patients with congenital adentia is undoubtedly an advantage of autologous dental transplantation [14—19], which, according to the authors, can be performed in any age group [20]. Known that at the age of 8—12 years, children undergo an active process of formation of the apical part of the root and the neurovascular bundle.
Therefore, auto transplantation of those teeth that formed at least 2/3 or 3/4 of the final root length was preferred. If the process of root formation is not observed after tooth transplantation, but resorption, then endodontic treatment is performed to preserve the tooth [21—25].
Goal
Improvement of bone grafting of the upper jaw with simultaneous tooth auto transplantation for the rehabilitation of patients with congenital cleft of the upper lip, alveolar process and palate.
Materials and methods
From October 2017, 26 patients between the ages of 9 and 12 with congenital cleft upper lip, alveolar and palate treated at the clinic of maxillofacial surgery of Moscow Regional Research and Clinical Institute. According to the history, clinical-laboratory examination and cone-beam computed tomography (CBCT) determined the volume of defect in the cleft area of the upper jaw.
After a consultation with an orthodontist, the indications for extraction of the donor tooth 4.4 were determined and a decision made to perform bone grafting of the upper jaw with simultaneous autologous tooth transplantation.
The patient had no contraindications. Written informed consent for surgical treatment obtained for the implementation of operational measures.
During bone grafting of the alveolar process of the upper jaw, surgical intervention performed in the volume: suturing of the oronasal anastomosis, fixation of fragments of the upper jaw with mini-plates and autotransplantation of the tooth. To fill the residual volume of the bone, a bone-plastic mixture used, obtained by mixing xenogenic bone material and auto-chips [26] taken with a bone scraper. The above osteoplastic mixture treated with an autologous conditioned plasma and isolated from the surrounding tissue resorbable and euromembrane [27]. After surgery, X-ray control was performed at 1, 3, 6 and 12 months to monitor the formation of the volume of bone structures and the apical part of the roots of autotransplanted teeth.
Clinical case
The clinic visited by patient B. 11 years old. With complaints, according to the mother, about the presence of a cleft in the alveolar process, food entering the nose. With the diagnosis: congenital complete right-sided cleft of the upper lip, alveolar process and palate. Congenital dental adentia 2.2, 2.4, dystopia, tooth retention 1.2. Condition after cheilorinoplasty (2006), uranoplasty (2006) and orthodontic treatment for 19 months (on braces).
On examination: the configuration of the face not changed, a normotrophic postoperative scar visualized on the skin of the upper lip. There is a deformation and flattening of the nose wing on the right. Opening of the mouth is free, in full. In the mouth: there is a complete cleft of the alveolar process of the maxilla in region of teeth 1.1—1.3, the diastasis between the fragments of the upper jaw and 4 mm, edentulous teeth 2.2, 2.4 (Fig. 1).
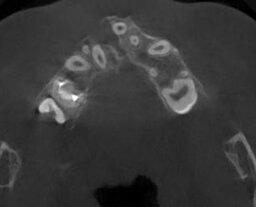
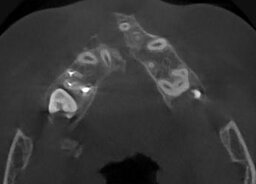
The results of CT-scan marked diastasis between the fragments of the upper jaw 13 mm, a bony defect in the alveolar bone basis and the pear-shaped hole on the right (Fig. 2).
The patient has a violation of the dentition formed mesial bite and indications for removal of the lower premolars (crowding of the lower teeth) according to the conclusion of the orthodontist.
The patient shown surgical intervention in the volume of bone grafting with simultaneous autotransplantation of the tooth 4.4 to the tooth area 1.2.
Complex treatment recommended:
- Conducting professional hygiene
- Orthodontic treatment
- Surgical intervention aimed at stabilizing fragments of the upper jaw, restoring the alveolar process, dentition.
Surgical stage
Scope of intervention: suturing of the oronasal anastomosis, stabilization of upper jaw fragments with miniplates, restoration of the alveolar process and dentition bone grafting of the alveolar process performed using a bone-plastic mixture consisting of auto- and xenomaterials with simultaneous autologous tooth transplantation.
Surgical intervention of bone grafting of the alveolar process of the upper jaw with simultaneous autotransplantation of the tooth.
Under endotracheal anesthesia, the mucous membrane of the alveolar process was incised in the area of teeth 1.4—2.3, the edges of the cleft were refreshed, mucoperiosteal flaps were detached from the vestibular and Palatine sides of the alveolar process, for maximum visualization of the surgical field.
After visualization of the defect area, dystopian and retinated tooth germ 1.2, the area of the oronasal anastomosis, the anastomosis was plasticized, the tooth germ 1.2 extracted, followed by immersion in saline solution (Fig. 3).
The area of the defect of the alveolar process from the soft tissues of the nasal cavity isolated by an automembrane. Miniplates used to fix fragments of the upper jaw with an overlap of the defect area of at least 0.5 mm with the help of a bone scraper, the edges of the bone defect not only refreshed, autogenic bone chips were taken from the oblique line of the lower jaw, followed by mixing with xenogenic osteoplastic material in a combination of 2:1. The donor tooth was collected 4.4 and placed in the cleft area (tooth 1.2).
The residual volume filled with a bone-plastic mixture and impregnated with autoplasm obtained by centrifugation according to the standard method of Dr. Joseph Choukroun. Osteoplastic mixture covered with resorbable membrane and euromembrane. In the area of the tooth 2.2 with the help of a cutter, a hole is formed in which the rudiment of the tooth 1.2 is installed (Fig. 4).
The Mucoperiosteal flaps mobilized, laid and sutured with nodular sutures by Vicril 4.0. Transplanted teeth fixed to the adjacent teeth using a retainer.
The postoperative period was uneventful. On the 7th day after the operation, the sutures removed and the patient discharged under the supervision of a dental surgeon at the place of residence. After 1 and 3 months after the operation, the patient did not complain at the control examination. The orthopantomogram images showed the preservation of the volume of bone regenerate. Absence of resorption of the root part of the transplanted teeth (Fig. 5, 6).
6 and 12 months after surgery, the patient did not complain.
The control CBCT [28, 29] noted the preservation of bone regenerative regeneration continued the formation of the apical part of the tooth, the absence of resorption of the root part of transplanted teeth 1.2, 2.1 and bone regenerate (Fig. 7, 8). The condition of the soft tissues of the palate and gums in the mouth is satisfactory, soreness and swelling is not noted. The patient is at the stage of orthodontic treatment (Fig. 9, 10).
Conclusions
Known that reconstructive surgery with the use of autobone is the “gold standard” [30]. Currently, modern biomaterials of natural or synthetic origin, which are able to influence osteogenesis, enhancing reparative processes in bone tissue, are successfully used in the maxillofacial region to restore the volume of lost bone structures and as a result of congenital malformations.
Thus, the clinical results showed that the postoperative evaluation of the bone structure after the plasticity of the alveolar process with instant autologous tooth transplantation and fixation of fragments of the upper jaw with the help of miniplates significantly reduces the surgical stages of rehabilitation of patients with congenital cleft upper lip and palate.
That ensures the projected recovery of the volume of alveolar growth and the recovery of the dental series.
Figures





References
- Haj M., Koudstaal M.J., Ramcharan M.S., Hoogeboom A.J.M., Koster M.P.H., Srebniak M.I., Cohen-Overbeek T.E. Undetected anomalies in foetuses with a prenatal diagnosis of isolated cleft. — Int J Oral Maxillofac Surg. — 2020; 49 (12): 1576—83. PMID: 32546322
- Depla A.L., Breugem C.C., Horst C.M.A.M., de Heus R., Boogaard M.-J.H., Maas S.M., Pajkrt E., Bekker M.N. Polyhydramnios in isolated oral cleft pregnancies: incidence and outcome in a retrospective study. — Prenat Diagn. — 2017; 37 (2): 162—7. PMID: 27943390
- Tokarev P.V., Shulaev A.V., Saleev R.A., Tokareva L.V., Gajsina E.A. Use of the speech passport in rehabilitation of children with congenital maxillofacial malformations. — Actual Problems in Dentistry. — 2019, 2: 79—83 (In Russ.).
- Alperovich M., Frey J.D., Shetye P.R., Grayson B.H., Vyas R.M. Breast milk feeding rates in patients with cleft lip and palate at a North American Craniofacial Center. — Cleft Palate Craniofac J. — 2017; 54 (3): 334—7. PMID: 27043654
- Ivanov A.L., Reshetnyak E.I., Starikova N.V., Udalova N.V., Nadtochy A.G. Resorbable vs nonresorbable fixation in alveolar bone grafting in unilateral cleft lip and palate patients. — Stomatology. — 2018; 1: 40—6 (In Russ.).
- Natarajan M. Three-dimensional assessment of alveolar bone thickness in individuals with nonsyndromic unilateral cleft lip and palate. — Journal of Cleft Lip Palate and Craniofacial Anomalies. — 2018; 2: 128—9. DOI: 10.4103/jclpca.jclpca_14_18
- Arsenina O.I., Malashenkova E.I., Pashchenko S.A. Algorithm of orthodontic treatment of cleft lip and palate patients before and after autogenous bone grafting. — Stomatology. — 2017; 5: 62—5 (In Russ.).
- Shetye P.R. Orthodontic management of patients with cleft lip and palate. — APOS Trends in Orthodontics. — 2016; 6: 281—6. DOI: 10.4103/2321—1407.194790
- Ushnitsky I.D., Isakov l.O., Vinokurov M.M., Oskol‘sky G.I. Structure and dynamics of congenital maxillofacial malformation in Yakutiya region. — Stomatology. — 2015; 2: 37—9 (In Russ.).
- Jafarova S.M. Medical and social rehabilitation of children with congenital cleft upper lip and palate. — In Proceedings of the XI international conference “Scientific dialogue: Questions of medicine”. — Saint-Petersburg: Social Science, 2017. — Pp. 4—10 (In Russ.).
- Rychlik D., Wójcicki P. Bone graft healing in alveolar osteoplasty in patients with unilateral lip, alveolar process, and palate clefts. — J Craniofac Surg. — 2012; 23 (1): 118—23. PMID: 22337386
- Hadler-Olsen S., Pirttiniemi P., Kerosuo H., Limchaichana N.B., Pesonen P., Kallio-Pulkkinen S., Lähdesmäki R. Root resorptions related to ectopic and normal eruption of maxillary canine teeth — A 3D study. — Acta Odontol Scand. — 2015; 73 (8): 609—15. PMID: 25891229
- Sugai T., Yoshizawa M., Kobayashi T., Ono K., Takagi R., Kitamura N., Okiji T., Saito C. Clinical study on prognostic factors for autotransplantation of teeth with complete root formation. — Int J Oral Maxillofac Surg. — 2010; 39 (12): 1193—203. PMID: 20630706
- Kvint S., Lindsten R., Magnusson A., Nilsson P., Bjerklin K. Autotransplantation of teeth in 215 patients. A follow-up study. — Angle Orthod. — 2010; 80 (3): 446—51. PMID: 20050735
- Bae J.-H., Choi Y.-H., Cho B.-H., Kim Y.-K., Kim S.-G. Autotransplantation of teeth with complete root formation: a case series. — J Endod. — 2010; 36 (8): 1422—6. PMID: 20647110
- Almpani K., Papageorgiou S.N., Papadopoulos M.A. Autotransplantation of teeth in humans: a systematic review and meta-analysis. — Clin Oral Investig. — 2015; 19 (6): 1157—79. PMID: 25903060
- Rohof E.C.M., Kerdijk W., Jansma J., Livas C., Ren Y. Autotransplantation of teeth with incomplete root formation: a systematic review and meta-analysis. — Clin Oral Investig. — 2018; 22 (4): 1613—24. PMID: 29525924
- Atala-Acevedo C., Abarca J., Martínez-Zapata M.J., Díaz J., Olate S., Zaror C. Success rate of autotransplantation of teeth with an open apex: Systematic review and meta-analysis. — J Oral Maxillofac Surg. — 2017; 75 (1): 35—50. PMID: 27725103
- Herford A.S., Nguyen K., Rojhani A. Alveolar ridge augmentation: An algorithmic approach. — In: Tolstunov L. (ed.). Horizontal alveolar ridge augmentation in implant dentistry: A surgical manual. — John Wiley & Sons, 2016. — Pp. 81—92. DOI: 10.1002/9781119019916.ch08
- Tanaka H., Toyoshima T., Atsuta I., Ayukawa Y., Sasaki M., Matsushita Y., Hiraoka R., Koyano K., Nakamura S. Additional effects of platelet-rich fibrin on bone regeneration in sinus augmentation with deproteinized bovine bone mineral: Preliminary results. — Implant Dent. — 2015; 24 (6): 669—74. PMID: 26204169
- Sakio R., Sakamoto Y., Ogata H., Sakamoto T., Ishii T., Kishi K. Effect of platelet-rich plasma on bone grafting of alveolar clefts. — J Craniofac Surg. — 2017; 28 (2): 486—8. PMID: 28033193
- Bagdadi K.E., Kubesch A., Yu X., Al-Maawi S., Orlowska A., Dias A., Booms P., Dohle E., Sader R., Kirkpatrick C.J., Choukroun J., Ghanaati S. Reduction of relative centrifugal forces increases growth factor release within solid platelet-rich-fibrin (PRF)-based matrices: a proof of concept of LSCC (low speed centrifugation concept). — Eur J Trauma Emerg Surg. — 2019; 45 (3): 467—79. PMID: 28324162
- Fortunato T.M., Beltrami C., Emanueli C., De Bank P.A., Pula G. Platelet lysate gel and endothelial progenitors stimulate microvascular network formation in vitro: tissue engineering implications. — Sci Rep. — 2016; 6: 25326. PMID: 27141997
- Morimoto N., Kakudo N., Ogura T., Hara T., Matsui M., Yamamoto M., Tabata Y., Kusumoto K. Easy-to-use preservation and application of platelet-rich plasma in combination wound therapy with a gelatin sheet and freeze-dried platelet-rich plasma: A case report. — Eplasty. — 2016; 16: e22. PMID: 27555889
- Sivarajasingam V., Pell G., Morse M., Shepherd J.P. Secondary bone grafting of alveolar clefts: a densitometric comparison of iliac crest and tibial bone grafts. — Cleft Palate Craniofac J. — 2001; 38 (1): 11—4. PMID: 11204675
- Miron R.J., Zucchelli G., Pikos M.A., Salama M., Lee S., Guillemette V., Fujioka-Kobayashi M., Bishara M., Zhang Y., Wang H.-L., Chandad F., Nacopoulos C., Simonpieri A., Aalam A.A., Felice P., Sammartino G., Ghanaati S., Hernandez M.A., Choukroun J. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. — Clin Oral Investig. — 2017; 21 (6): 1913—27. PMID: 28551729
- Amirlak B., Tang C.J., Becker D., Palomo J.M., Gosain A.K. Volumetric analysis of simulated alveolar cleft defects and bone grafts using cone beam computed tomography. — Plast Reconstr Surg. — 2013; 131 (4): 854—9. PMID: 23542257
- Oh T.S., Park J.S., Choi J.W., Kwon S.M., Koh K.S. Risk factor analysis of bone resorption following secondary alveolar bone grafting using three-dimensional computed tomography. — J Plast Reconstr Aesthet Surg. — 2016; 69 (4): 487—92. PMID: 26718845
- Ivanov S.Yu., Bizyaev A.F., Lomakin M.V., Panin A.M. Dental Implantology. — Moscow: Russian Ministry of Health, 2000. — 96 p. (In Russ.).
- Ivanov S.Iu., Iamurkova N.F., Muraev A.A. Defect elimination of mandible alveolar part by sandwich plastics. — Stomatology. — 2010; 2: 42—7 (In Russ.).