DOI:
10.37988/1811-153X_2021_4_62Phlegmon of the oral floor and deep spaces of the neck, complicated by sepsis: A clinical case
Downloads
Abstract
Ludwig’s angina is a life-threatening condition of a purulent inflammatory nature, accompanied by diffuse cellulite of the soft tissues of the muscular floor of the oral cavity and neck. The title comes from the name of german physician Wilhelm Friedrich von Ludwig, who first described it in 1836. It includes three sections of the muscular floor of the oral cavity: the sublingual, submental and submandibular. Early detection and treatment, including airway protection, surgery, wound drainage, and adequate antibiotic therapy, are critical. The primary task in pyogenic inflammatory diseases of the maxillofacial region is to create an optimal outflow for the inflammatory exudate. The article presents a clinical case of a 40-year-old patient with diffuse phlegmon of the floor of the mouth with spread to the deep cellular spaces of the neck on both sides, complicated by sepsis. According to the patient, about 1 month ago (05/09/2021), aching pain appeared in the area of the tooth 4.8. After 5 days, she noticed pain when biting on a tooth 4.8. She did not seek help, she was self-medicating, aimed at eliminating the pain syndrome. After 2 weeks (05/23/2021) pain in tooth 4.8 disappeared, edema appeared in the submandibular region on the right. Against the background of self-medication, negative dynamics was noted. 06/08/21 the patient was hospitalized in the department of maxillofacial surgery, where surgical and drug treatment was prescribed. After the complete relief of inflammatory manifestations, on the 22nd day from the moment of admission to the hospital (06/30/21), lamellar sutures were imposed, which were removed after 10 days. The wound healing was uneventful. During her stay in the hospital, a physician of physical therapy (exercise therapy) worked with the patient, as a result of which it was possible to restore the swallowing function and remove the nasogastric tube. On the 39th day (July 17, 2021), she was discharged for outpatient follow-up care at a dentist-surgeon and exercise therapy doctor at the place of residence.Key words:
purulent-inflammatory diseases, maxillofacial region, phlegmon of the muscular floor of the oral cavity, phlegmon of the neck, sepsisFor Citation
Introduction
Despite the advances achieved in the diagnosis and treatment of pyoinflammatory diseases of the maxillofacial region (MFR), they continue to be the most difficult problem in maxillofacial surgery (MFS). Today, in our country, this pathology remains the most common form of septic inflammation. Among the reasons are odontogenic [1] and non-odontogenic, complicated by immunodeficiencies of various etiologies. Late seeking dental care, due to both psychological and socio-economic factors, and territorial, associated with the low availability of qualified care, untimely assistance, and sometimes even the wrong tactics of treating odontogenic diseases at the primary admission in outpatient facilities lead patients to long-term treatment in maxillofacial hospitals, often in intensive care.
According to various sources, every year from 0.1 to 0.3% of patients from the total number of patients admitted to hospitals in the Russian Federation die from purulent-inflammatory diseases of the maxillofacial region [2]. Among all phlegmon of the maxillofacial region one located in the floor of the oral cavity occurs more often than other localizations [3].
As it is know, phlegmon of the floor of the mouth, or Ludwig's angina, is a diffuse cellulite in the submandibular, sublingual and submental spaces, characterized by a tendency to rapidly spread to the surrounding tissues [4]. Early recognition and treatment of Ludwig's angina is of paramount importance due to the high risk of systemic complications: due to rupture of the carotid artery or abscess of the carotid vagina, thrombophlebitis of the internal jugular vein, mediastinitis, empyema, osteomyelitis of the mandible, subphrenic abscess, aspiration pneumonia and pleural effusion [5]. Clinical signs may include life-threatening symptoms such as bilateral edema, dysphagia, profuse drooling, neck tenderness, tongue elevation and edema, trismus, dyspnea and stridor, which can lead to airway obstruction [6]. Numerous studies and case reports indicate that CT scanning is preferable for patients who may be in a horizontal position [7, 8].
It should be noted the importance of knowledge of the topographic and anatomical features of the neck, since marking the external anatomical landmarks of the airways before manipulating them can save vital time [6].
The aim was to present a clinical case of inflammation of the deep cellular spaces of the neck on both sides, complicated by serous mediastinitis.
Clinical case
Patient H., 40 years old, was taken by an ambulance team from the dental clinic to the maxillofacial department with a diagnosis of facial phlegmon.
Anamnesis of the disease: according to the patient, about 1 month ago (at the beginning of May 2021) there was aching pain in the area of the tooth 4.8. After 5 days, she noted pain when biting on a tooth 4.8. She did not seek help, she self-medicated, aimed at eliminating the pain syndrome. After 2 weeks, the pain in tooth 4.8 disappeared, edema appeared in the submandibular region on the right. Applied alcohol solutions, after which the edema increased in size. She did not seek help, continued to be treated on her own. For the next 2 weeks, negative dynamics was noted in the form of an increase in edema, its spread to the submental and submandibular region from the opposite side, the appearance of puffiness in the neck on both sides, and hyperemia of the skin. In early June 2021, the pain syndrome intensified, weakness appeared, the body temperature rose to 39.0° C, in connection with which the patient turned to a dental clinic for help, where she was examined by a dentist-surgeon and sent to the maxillofacial department.
Objective status: an external examination revealed a violation of the configuration of the face due to edema in the lower third of the buccal region on the right, submandibular and submental regions with extension to the lateral and anterior surfaces of the neck from both sides to the level of the jugular notch. The skin in the submandibular region and in the upper-lateral part of the neck on the right is slightly hyperemic, tense, and does not fold into a fold. Palpation revealed acute pain in the submandibular, submental areas, as well as on the inner surface of the lower jaw angle on the right (in the projection of the attachment of the medial pterygoid muscle to the lower jaw). Soreness along the anterior edge of the sternocleidomastoid muscles on both sides, mainly on the right. Opening the mouth up to 1 cm, examination of the oral cavity is difficult.
In the oral cavity, there was edema of the sublingual ridges on both sides, the mucous membrane was hyperemic, fibrin plaque (mainly on the right). The tongue is raised due to edema of the hyoid ridges, palpation of the tongue is painless, movements are preserved in full. The pterygomandibular fold on the right is edematous, hyperemic. Asymmetry of the pharynx due to edema of the lateral surface of the pharynx on the right. The crown of the 4.8 tooth is destroyed by 2/3 by a carious process. The surrounding mucous membrane is hyperemic, edematous. Purulent discharge from the periodontal junction. Percussion of the 4.8 tooth was painful. Considering the clinical symptoms, the patient underwent examination, including general and biochemical blood tests, coagulogram, electrocardiography, multislice computed tomography (MSCT) of the facial skeleton, neck and chest.
According to the results of the examination, the diagnosis was made: diffuse putrefactive-necrotic phlegmon of the bottom of the oral cavity, pterygomandibular, peripharyngeal spaces on the right, deep cellular tissue spaces of the neck on both sides.
Under the endotracheal general anesthesia was performed an incision in the submandibular region on the right, parallel to the edge of the mandible from the its corner on the right to the angle of the opposite side. Layer-by-layer soft tissues were dissected, revision of the submandibular region, pterygomandibular, peripharyngeal spaces on the right was carried out, the diaphragm of the floor of the oral cavity was cut off, then the anterior abdomens of the digastric muscles and the sublingual muscles were transected on both sides, the submandibular region was revised on the left, the sublingual muscle was cut off from the bone. on the left — a large amount of purulent discharge was obtained in all of the listed spaces. A smear was taken to determine the microflora and antibiotic sensitivity. When revising the pterygomandibular, peripharyngeal spaces on the left, free pus was not obtained. Together with the surgeons, an opening of the deep cellular spaces of the neck was performed on both sides — a purulent discharge was obtained (more on the right). Drainage of the revised cellular tissue spaces with glove graduates and half-pipe drains (for the formation of wound channels and adequate outflow of inflammatory exudate) was performed.
Treatment
Taking into the diffuse nature of the purulent-inflammatory process, as well as the volume of surgical intervention, after opening the purulent focus, the patient was transferred to the Department of anesthesiology and resuscitation for further treatment and observation. Extubation was not performed due to upper airway edema.
Empiric antibiotic therapy was prescribed: vancomycin, 1 g 2 times a day, intravenously, drip. no. 10; invanz, 1000 mg 1 time, intravenous drip. no. 10. Prescribed parenteral and tube feeding through a nasogastric tube. Wound dressings were performed daily, 2 times a day.
The first analysis of the microbiological landscape showed the presence of Streptococcus spp. anhaemolyticus — 107 CFU/ml, Streptococcus spp. haemolyticus — 107 CFU/ml, anaerobic microflora was not isolated.
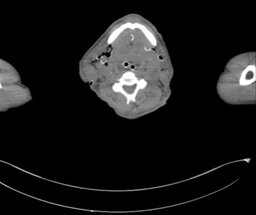
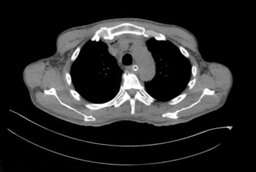
In order to control the quality of treatment in dynamics, MSCT of the facial skeleton, neck and chest organs was performed, signs of descending mediastinitis were revealed (Fig. 1, 2).
Description of MSCT dated 06/10/2021: in the dynamics of the state after surgical interventions on the submandibular regions and soft tissues of the neck — were found the massive wound defects, drainages, edema and gas bubbles are visible, no clear signs of delimited fluid accumulations. Also the edema and infiltration of tissue spreads into the upper mediastinum 2 cm below the notch of the sternum handle, into the anterior section and paratracheal, more gas bubbles spread to the right and no registration of the accumulations of liquid. The mediastinum is not displaced, the lymph nodes are not enlarged. The trachea is not displaced. In the posterior cortical regions of the lungs, the pulmonary pattern thickened, there are no focal and infiltrative changes. Bronchi 1—3 orders of magnitude passable.
Thoracoscopy was performed (was used general endotracheal anesthesia) together with surgeons, according to the results of which swelling of the soft tissues of the anterior superior mediastinum was determined, without the presence of exudate. Drainages for active aspiration are installed in the mediastinum.
Considering the large amount of purulent discharge from the wound and the absence of positive dynamics in the form of a decrease in edema, the patient underwent dressing of the wound under anesthesia: the revision of the previously disclosed cellular spaces was repeated. During that no delimited accumulations of pus were found. New drains were installed in the wound. Re-dressing under anesthesia was performed on June 15, 2021. Before revision of the wound, was performed the MSCT of the facial skeleton, neck and chest organs, according to which positive dynamics was noted in the form of a decrease in edema and the amount of free exudate in the area of the floor of the mouth and neck. During dressing under anesthesia, necrectomy of non-viable areas of soft tissues was performed, a smear was taken again to determine microflora and sensitivity to antibiotics, and drainages from the mediastinum were removed.
Sowing of microflora from 06/15/2021: Enterococcus faecalis — 10 CFU/ml, Escherichia coli — 10 CFU/ml, Staphylococcus haemolyticus — 103 CFU/ml, anaerobic flora is not isolated. Then the antibacterial drugs were replaced with gentamicin 240 mg once a day, intravenously, fosfomycin 2 g 3 times a day, intravenously.
In view of the presence of positive dynamics in the form of a decrease in edema, the nasogastric tube was removed, and attempts were made to feed the patient enterally.
06/22/2021 transferred for further treatment from the Department of anesthesiology and resuscitation to the Department of maxillofacial surgery. Due to the complete cutting off of the anterior venters of the digastric and mylohyoid, the patient's swallowing function is significantly impaired. A nasogastric tube is reinstalled for nutrition. Dressings were performed daily, once a day. On the 8th day of being in the maxillofacial surgery department, the wound cleared, the process of scarring began, as a result of which the musculocutaneous flap on the neck shrank, forming a pronounced diastasis of the wound edges (Fig. 3).
On June 30, 2021, button sutures were imposed, which were twisted every 2—3 days, pulling the wound edges towards each other (Fig. 4).
On the 10th day from the moment of imposition, the plate sutures were removed. The wound healing was uneventful. During her stay in the hospital patient got the physical therapy, as a result of which it was possible to restore the swallowing function and remove the nasogastric tube.
07/17/2021 was discharged for outpatient follow-up care at the dental office and rehabilitation therapy doctor at the place of residence (Fig. 5, 6).
Discussion
The condition for successful treatment of neck phlegmon are urgent surgical intervention and a wide opening and adequate drainage of the deep cellular tissue spaces of the neck [9].
It is necessary to draw the attention of novice specialists to the need for a thorough opening by layer-by-layer dissection of tissues and drainage of cavities to exclude the formation of purulent streaks. The literature has repeatedly raised the issue of optimal surgical approaches and adequate clinical situation of antibiotic therapy [10].
Treatment and rehabilitation of patients with phlegmon of the floor of the oral cavity should be carried out in close interdisciplinary contact between specialist doctors and nurses. However, it is important to consider the need for continuing education, awareness and competence of healthcare professionals to ensure successful diagnosis, management and treatment of this condition, especially in the context of patients with limited access to dental care who first visit the emergency department [11].
Conclusion
The correct choice of management tactics in the case of an advanced purulent-inflammatory process of the maxillofacial region plays an important role both in the treatment and in saving the patient's life.
Additional research methods facilitate differential diagnosis in the doctor's work, allowing to improve the quality of the treatment provided.
References
- Cousin G.C., Yousaf I. Ludwig’s angina: infected teeth must be extracted. BMJ. 2020; 371: m4466. PMID: 33208308
- Orazvaliev A.I., Dubov D.V., Vagner O.N. The Statistical analysis of the frequency and structure of purulent-inflammatory diseases of the maxillofacial region on the materials of the Department of Maxillofacial Surgery № 2 of Inozemtsev Municipal Clinical Hospital. Russian Stomatology. 2020; 13 (2): 12—5 (In Russ.). eLIBRARY ID: 42926971
- Shevchenko L.V., Pakhlevanyan S.G., Zhuravlev Yu.I. Purulent-inflammatory diseases of the maxillofacial region in patients with polymorbid conditions is a multidisciplinary problem (literature review). Belgorod State University Scientific bulletin: Medicine, Pharmacy. 2018; 41 (3): 436—48 (In Russ.). eLIBRARY ID: 36423978
- Miah M.R., Ali A.S. Ludwig’s angina. Br Dent J. 2020; 229 (5): 268. PMID: 32917993
- Pak S., Cha D., Meyer C., Dee C., Fershko A. Ludwig’s Angina. Cureus. 2017; 9 (8): e1588. PMID: 29062620
- Dowdy R.A.E., Emam H.A., Cornelius B.W. Ludwig’s angina: Anesthetic management. Anesth Prog. 2019; 66 (2): 103—110. PMID: 31184944
- Bridwell R., Gottlieb M., Koyfman A., Long B. Diagnosis and management of Ludwig’s angina: An evidence-based review. Am J Emerg Med. 2021; 41: 1—5. PMID: 33383265
- Kobayashi M., Watanabe K. Ludwig angina. CMAJ. 2017; 189 (6): E246. PMID: 27956390
- Paramonova O.A., Savchenko Ju.P., Gerbova T.V., Uvarova A.G. Modern techniques for face and neck phlegmons treatment. Kuban Scientific Medical Bulletin. 2018; 25 (5): 58—64 (In Russ.). eLIBRARY ID: 36289561
- Vallée M., Gaborit B., Meyer J., Malard O., Boutoille D., Raffi F., Espitalier F., Asseray N. Ludwig's angina: A diagnostic and surgical priority. Int J Infect Dis. 2020; 93: 160—2. PMID: 31981767
- Shemesh A., Yitzhak A., Ben Itzhak J., Azizi H., Solomonov M. Ludwig angina after first aid treatment: Possible etiologies and prevention—Case report. J Endod. 2019; 45 (1): 79—82. PMID: 30446404