DOI:
10.37988/1811-153X_2021_4_13Evaluation of enamel remineralization rate by quantitative light-induced fluorescence
Downloads
Abstract
Evaluation of the rate of remineralization of enamel in 15 teeth with initial caries on the vestibular surface of the frontal group of teeth after orthodontic treatment is considered.Materials and methods.
Remineralization rate was assessed by quantitative light-induced fluorescence using a Qraycam camera and accompanying software. Mean loss of mineral components (∆F), maximal loss of mineral components (∆Fmax), area of demineralization (WSA) and microbial activity in demineralization (∆R) were determined 1 week, 1 month and 1 year after removal of orthodontic appliances and without prescription of remineralizing agents.
Results.
At the beginning of the study, ∆F, ∆Fmax, ∆Q, and ∆R were 6.1%, 12.1%, 65.75 px, and 13.25%, respectively. One year later, these rates improved to 4.2%, 7.2%, 33.75 px, and 6%.
Conclusion.
After removal of the bracket system in patients with initial caries, natural enamel remineralization did not fully occur.
Key words:
enamel remineralization, Quantitative Light-induced Fluorescence, enamel demineralization diagnosisFor Citation
Introduction
According to studies, patients who are treated with removable and fixed orthodontic appliances have a very high risk of getting tooth decay. It can reach 100%, in addition. Also the number of patients receiving orthodontic treatment is constantly increasing.
Therefore, the issues of prevention and treatment of dental caries are still relevant [1—3].
The following reasons may be responsible for patients’ high prevalence of tooth decay:
- oral hygiene is worsened by orthodontic appliances;
- patients should brush their teeth after each meal and use extra hygiene items (interdental brushes, irrigators), but not all patients comply doctor's orders;
- teen-agers and children have difficulty complying with recommendations because they have busy school schedules and many after-school tutoring programs;
- orthodontic treatment takes a long time — it takes 16—24 month in common and takes 36 month in complex clinical cases [4];
- the orthodontist did not consider that the patient initially had little motivation for good oral hygiene
- patients with orthodontic appliances need oral hygiene at least twice a year.
Saliva is a natural source of remineralization for tooth enamel. Saliva is oversaturated with phosphorus and calcium ions. In saliva phosphate is contained in two forms — bound to protein and other compounds and free, ionized. In saliva, the content of total phosphate reaches 7 mmol/l. 70% is represented by inorganic phosphate. Inorganic phosphorus is represented by the ions HPO42− and H2PO4−, which form the phosphate buffer system. In saliva calcium content ranges from 1.0 to 3.0 mmol/l. Calcium is present in ionized form and combined with proteins as phosphates [5].
Calcium and phosphorus compounds saturate the enamel and maintain a balance in the processes of demineralization and remineralization
So we had a question: is saliva capable to saturate the enamel with calcium and phosphorus if we remove orthodontic appliances from patients who have white spots on dental hard tissues, what means we eliminate a risk factor of enamel demineralization?
Objectives
Determine if saliva can do remineralization of enamel after removal of orthodontic appliances using Quantitative Light-induced Fluorescence (QLF). Since the aim is to solve following challenges:
- Carry out a study patients white spots of demineralization using QLF.
- To examine the changes of average mineral loss, maximum mineral loss, white spots area and bacteria activity in white spots after a 1, 4 and 52 weeks using QLF.
- Define could saliva remineralize enamel physiologically while risk factors were eliminated (dental plaque accumulation).
Materials and methods
So far dentists has many techniques and tools to detect caries at all stages of development. The most common method to detect caries is still tooth visual examination [6—8]. ICDAS (Caries Detection and Assessment System) was created by research team. It has high sensitivity, specificity as radiology and laser fluorescence [9]. Also the ICDAS-II-SSC — International caries detection and assessment system for the smooth surface, a new specific system of initial caries detection is accurate as radiology [10]. The latest one is still the most accurate for initial caries detection on occlusal and approximate surfaces [11—13].
Laser fluorescence is an optical method of caries detection and very common because of it simplicity and high precision [14, 15]. The combination of the above-mentioned methods are ensure the most accurate results for detection initial caries and its development [16, 17].
However, the above-mentioned methods are effective for initial caries detection, but they don’t approach for measuring effectiveness — it impossible to monitor the development of caries lesion. So what will help a dentist to measure the effectiveness of remineralization therapy?
Staining initial caries by 2% methylene blue solution using the Axamit scale during remineralization therapy is the most common method to define a loss depth, but it hard to measure white spots area changing because a graph paper is needed.
Measure calcium and phosphorus in enamel ash in vitro is technically hard to reproduce and can not be possible on clinical practice [18]. Also using electron microscope is possibly only in laboratory [19].
Taking a photo of teeth and highlighting white spots to compare it before and after therapy in special programs also recommended. Unfortunately that method is not sufficiently objective because results depend from quality of photos and it couldn’t be used at scientific study.
QLF for early caries diagnosis also applies today. This method was discovered in 1980 and has been enhanced over time. Today initial caries cannot be only detected but also examined by software [20].
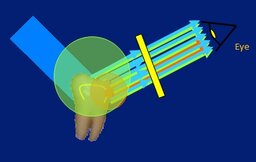
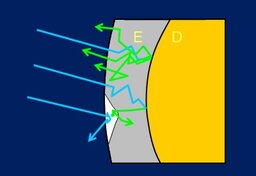
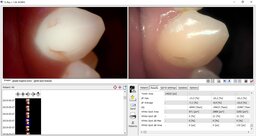
QLF is based on dental hard tissue light reflection (Fig. 1). Unharmed enamel reflect light fully (Fig. 2). Enamel with caries lesion has microcavities what absorb light. A light — reflected and absorbed — is analyzed by the software and shows (Fig. 3):
- average mineral loss (ΔF);
- maximum mineral loss (ΔFmax);
- white spots area;
- bacteria activity in caries lesion (ΔR).
Qraycam’s light is absolutely safe for body (420—480 nm) so the method cam be used in clinical practice in vivo. The effectiveness of remineralization therapy and caries lesion management could be monitoring by QLF [21—23]. We acknowledge that as the most safe, specific, quick, technically available method of caries detection [24, 25].
Our team examined 15 teeth from 5 patients with initial caries on vestibular and lingual surfaces after brackets debonding by QLF. Adhesive materials leftovers were removed by polishing heads Enhance (Dentsply), professional hygiene with Clean Polish (Kerr) toothpaste and brush was made after orthodontics appliance debonding. Also using fluoride free toothpastes was recommended to patients.
White spots were examined by Qraycam™ (AIOBIO, S. Korea; Fig. 4) and next parameters were assessed on each visit after 1, 4 and 52 weeks: average mineral loss (ΔF); maximum mineral loss (ΔFmax); white spots area; bacteria activity in caries lesion (ΔR).
Results and discussion
Average mineral loss ∆F of initial caries on vestibular and lingual surfaces after orthodontics treatment has a progress from −6.1% to −4.8%, and became −4.2% after a year (+31%, see table).
Maximum mineral loss also ∆Fmax has a progress from −12.1% to −7.2% after a year (+40%, see the table and Fig. 5).
White spots area also decrease through year: average value of white spots area was 65.75 pixel in the beginning of study and became 33.75 pixel in the end (+49%).
| Parameter | Time, weeks | ||
| 1 | 4 | 52 | |
| ∆F (%) | −6.1 | −4.8 | −4.2 |
| ∆Fmax (%) | −12.1 | −9.6 | −7.2 |
| WSA (px) | 65.75 | 57.00 | 33.75 |
| ∆R (%) | 13.25 | 10.50 | 6.00 |
Conclusions
QLF is a good method to monitor initial caries management — a quantity of mineral loss in demineralization spot — in vivo. It is preferably on clinical practice. Also it provide to measure white spots area and bacteria activity in caries loss.
Considering a progress of initial caries management by QLF is observed that the average mineral loss ∆F in the beginning of study was −6.1% and became −4.2% after a year. Maximum mineral loss ∆Fmax was −12.1% and increased to −7.2%; white spot area ∆Q was 65.75 and decreased to 33.75; bacteria activity in caries lesion was 13.25% and became 6%.
According to our study saliva with calcium and phosphate ions couldn’t remineralize initial caries spots on enamel after orthodontics treatment fully.
References
- Gorelick L., Geiger A.M., Gwinnett A.J. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982; 81 (2): 93—8. PMID: 6758594
- Yli-Junnila P., Kuusisto H., Kuivanen A., Karhuvaara R., Istrefi A., Peltomaa J. Treatment of caries in a spot stage at the patients who finished orthodontic treatment on a bracket-system. Pediatric Dentistry and Profilaxis. 2018; 18 (5): 19—23 (In Russ.). eLIBRARY ID: 37027436
- Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod. 1992; 19 (3): 199—205. PMID: 1390575
- Gorlacheva T.V., Terekhova T.N. Duration of orthodontic treatment with extractions of the teeth. In: Proceedings of the “Parin Readings 2018” congress. Minsk: Belorussia State University, 2018. Pp. 210—213 (In Russ.).
- Kosyuga S.Y., Botova D.I. Dynamics of the intensity of dental caries in patients with permanent orthodontic constructions. Medical Council. 2017; 5: 191—192 (In Russ.). eLIBRARY ID: 29186340
- Braga M.M., Oliveira L.B., Bonini G.A., Bönecker M., Mendes F.M. Feasibility of the International Caries Detection and Assessment System (ICDAS-II) in epidemiological surveys and comparability with standard World Health Organization criteria. Caries Res. 2009; 43 (4): 245—9. PMID: 19439944
- Chu C.H., Chau A.M., Lo E.C. Current and future research in diagnostic criteria and evaluation of caries detection methods. Oral Health Prev Dent. 2013; 11 (2): 181—9. PMID: 23534041
- Dikmen B. ICDAS II criteria (international caries detection and assessment system). J Istanb Univ Fac Dent. 2015; 49 (3): 63—72. PMID: 28955548
- Rodrigues J.A., Hug I., Diniz M.B., Lussi A. Performance of fluorescence methods, radiographic examination and ICDAS II on occlusal surfaces in vitro. Caries Res. 2008; 42 (4): 297—304. PMID: 18663299
- Vaswani S., Sharma D.S., Mishra S., Sharma S. Histologic validation of ICDAS-II and polarization sensitive optical coherence tomography to detect smooth surface early carious lesions. Int J Paediatr Dent. 2018; 1—10. PMID: 30387228
- Keenan J.R., Keenan A.V. Accuracy of dental radiographs for caries detection. Evid Based Dent. 2016; 17 (2): 43. PMID: 27339235
- Wenzel A., Larsen M.J., Fejerskov O. Detection of occlusal caries without cavitation by visual inspection, film radiographs, xeroradiographs, and digitized radiographs. Caries Res. 1991; 25 (5): 365—71. PMID: 1747887
- Schwendicke F., Tzschoppe M., Paris S. Radiographic caries detection: A systematic review and meta-analysis. J Dent. 2015; 43 (8): 924—33. PMID: 25724114
- Tassoker M., Ozcan S., Karabekiroglu S. Occlusal caries detection and diagnosis using visual ICDAS criteria, laser fluorescence measurements, and near-infrared light transillumination images. Med Princ Pract. 2020; 29 (1): 25—31. PMID: 31158839
- Shi X.Q., Welander U., Angmar-Månsson B. Occlusal caries detection with KaVo DIAGNOdent and radiography: an in vitro comparison. Caries Res. 2000; 34 (2): 151—8. PMID: 10773633
- Melo M., Pascual A., Camps I., Del Campo Á. In vivo study of different methods for diagnosing pit and fissure caries. J Clin Exp Dent. 2015; 7 (3): e387—91. PMID: 26330935
- Valera F.B., Pessan J.P., Valera R.C., Mondelli J., Percinoto C. Comparison of visual inspection, radiographic examination, laser fluorescence and their combinations on treatment decisions for occlusal surfaces. Am J Dent. 2008; 21 (1): 25—9. PMID: 18435372
- Golovanenko A.L., Tretyakova E.V., Patlusova E.S., Alekseeva I.V., Berezina E.S., Pershina R.G. Study of remineralizing activity of dosage forms for treatment of initial enamel caries. Pharmacy & Pharmacology. 2018; 6 (4): 380—388 (In Russ.). eLIBRARY ID: 35564873
- Vyavhare S., Sharma D.S., Kulkarni V.K. Effect of three different pastes on remineralization of initial enamel lesion: an in vitro study. J Clin Pediatr Dent. 2015; 39 (2): 149—60. PMID: 25823485
- Park S.W., Kim S.K., Lee H.S., Lee E.S., de Josselin de Jong E., Kim B.I. Comparison of fluorescence parameters between three generations of QLF devices for detecting enamel caries in vitro and on smooth surfaces. Photodiagnosis Photodyn Ther. 2019; 25: 142—147. PMID: 30508664
- Günther E., Park K.J., Meißner T., Kottmann T., Schmalz G., Haak R., Ziebolz D. Assessment of non-cavitated root caries lesions by quantitative light-induced fluorescence-An in vivo feasibility study. Photodiagnosis Photodyn Ther. 2020; 30: 101671. PMID: 31988025
- Jun M.K., Park S.W., Lee E.S., Kim B.R., Kim B.I. Diagnosis and management of cracked tooth by quantitative light-induced fluorescence technology. Photodiagnosis Photodyn Ther. 2019; 26: 324—326. PMID: 31042556
- Shi X.Q., Tranaeus S., Angmar-Månsson B. Comparison of QLF and DIAGNOdent for quantification of smooth surface caries. Caries Res. 2001; 35 (1): 21—6. PMID: 11125192
- Kim E.S., Lee E.S., Kang S.M., Jung E.H., de Josselin de Jong E., Jung H.I., Kim B.I. A new screening method to detect proximal dental caries using fluorescence imaging. Photodiagnosis Photodyn Ther. 2017; 20: 257—262. PMID: 29079349
- Alammari M.R., Smith P.W., de Josselin de Jong E., Higham S.M. Quantitative light-induced fluorescence (QLF): a tool for early occlusal dental caries detection and supporting decision making in vivo. J Dent. 2013; 41 (2): 127—32. PMID: 22940557