Evaluation of the effectiveness of the use of collagen cones in the post-extraction socket preservation in patients on temporary antithrombotic therapy
Downloads
Abstract
When taking antiplatelet agents and anticoagulants, a change in the hemostatic properties of blood leads to a decrease in its viscosity and the adhesion strength of platelets, which is reflected in the slowing down of the formation of a blood clot and the likelihood of its detachment. The aim of this study was to study the effectiveness of the use of collagen cones for the socket preservation in patients temporarily receiving antithrombotic therapy.Materials and methods.
The pilot study, conducted from December 2020 to May 2021, included 27 patients. The main group consisted of 17 patients in need of surgical debridement of the oral cavity, aged 30 to 45 years, without a somatically burdened history, who underwent SARS CoV-2. The comparison group consisted of 10 people within the same age, but did not receive any medications on a regular basis. Collagen cones Alvokon were used to preserve alveolar sockets. To assess osteogenesis, all patients underwent X-ray examinations of the area of interest immediately after removal and after 1 month.
Results.
In patients of both groups, the density of the bone pattern in the area of interest increased, which indicates normal osteogenesis. However, in the patients of the main group, the bone density in the areas of interest comparable to the segments of the patients in the comparison group was slightly lower. Discussion. The results of the pilot study show the effectiveness of collagen cones not only as an osteoplastic material, but also as an excellent local hemostatic.
Conclusion.
Collagen cones are recommended for use in patients receiving antithrombotic therapy with selective inhibitors of coagulation factors Xa, in order to prevent the development of early and late local bleeding during surgical debridement of the oral cavity.
Key words:
direct oral anticoagulants, COVID-19, postextraction bleeding, postextraction preservation, collagen spongesFor Citation
Introduction
The standards for successful tooth extraction are considered not only surgical debridement of dental socket but also the preservation of the volume of the bone structures of the alveoli as well as minimal trauma to the keratinized gum zone [1, 2]. It is often performed simultaneous replacement of the defect with dental implants [3]. If there is a not enough of bone tissue to restore the height and thickness of the alveolar process after the tooth extraction procedure the hole is filled with an osteoplastic material with an overlap to seal the wound bed with a mucoperiosteal flap [4—8]. The most difficult in aesthetic surgical dentistry remains the replacement of the loss of bone tissue and surrounding soft tissue formations [1—3]. If no preventive dental measures are taken during the first year after tooth extraction bone resorption in the area of injury is up to 70% [9, 10]. At the same time the keratinized gum zone can completely disappear and the teeth roots adjacent to the defect are exposed provoking the sensitivity of these teeth and the formation of a recession. This leads to a pronounced change in tissues and with the subsequent introduction of dental implants into this zone deteriorates their stability, durability and aesthetics [3]. Methods of filling and sealing the sockets of removed teeth with special materials were developed to prevent bone atrophy and deformation of the alveolar ridge [1, 3, 4, 7, 11, 12].
Preservation of the alveolar socket allows preserving bone volume, area of the attached gum, gingival papillae, the size, shape and histological structure of which are important for the “red” (gum) aesthetics, reduces post extraction pain symptoms and the likelihood of alveolitis and reduces the healing period. Thus this makes it possible to make a dental implant at an earlier time or to prevent the loss of hard and soft tissues if the patient cannot undergo this procedure for some reason in the next six months [1, 7, 13].
The most common methods of socket preservation include the use of two components: a bone-forming substance with osteoconductive or inductive properties and a barrier coating of natural or artificial origin (free gingival graft, collagen membrane, mucoperiosteal flap, etc.) [1—4, 7, 8, 14].
In some people performing any surgical, including dental, manipulations is complicated by early or delayed bleeding, increasing the risk of socket infection and reducing the growth of bone tissue in the area of tooth extraction.
A high risk of hemorrhagic complications after invasive dental procedures occurs in patients receiving antiplatelet and anticoagulant therapy [15—18]. Currently because of the SARS CoV-2 Coronavirus pandemic the number of patients temporarily receiving such therapy has increased dramatically [19, 20].
Collagen is a necessary substrate for the formation of a platelet-fibrin clot. The cone shape is convenient to use, contributes to the prevention and treatment of alveolitis, as well as the socket safety for subsequent dental implantation. Today the following combinations of drugs can be found in Russia as part of Alvokon collagen cones: Alvokon collagen sponge No. 3 — collagen, lidocaine, chlorhexidine bigluconate, calcium hydroxyapatite, and Alvokon collagen sponge No. 5 — collagen, calcium hydroxyapatite, iodoform, metronidazole.
In normal conditions the produced collagen is sufficient to stop bleeding. However if taking antiplatelet agents and anticoagulants a change in the hemostatic properties of blood leads to a decrease in its viscosity and platelet adhesion strength that affects the slowing down of the formation of a blood clot and the likelihood of its separation [21, 22].
The aim of study was to investigate the effectiveness of collagen cones for the socket preservation in patients temporarily receiving antithrombotic therapy.
Materials and methods
The pilot study from December 2020 to May 2021 included 27 patients. Patients were informed about the methods of treatment, inclusion in the clinical study and filled out and signed an informed consent.
All patients were divided into 2 groups. The main group consisted of 17 patients aged 30 to 45 years old who needed surgical debridement of the oral cavity without severe comorbidities who had SARS CoV-2 infection from 1 to 3 months before they went to dentist. To prevent thrombotic complications patients: 8 (47%) men and 9 (53%) women, received antithrombotic drugs in tablet form: Rivaroxaban 20 mg per day: 5 women and 4 men or Apixaban 2.5 mg 2 times a day: 4 women and 4 men. Comparison group included 10 patients (5 women and 5 men) within the same age but who did not receive medications on a regular basis.
Patients of both groups underwent tooth extraction due to acute or exacerbation of chronic periodontitis. Oral hygiene of all participants in the pilot study was satisfactory. The removal of teeth was performed for all participants using Luxator’s to minimize tissue injury. The drug of choice for local anesthesia was a 4% solution of articaine with epinephrine 1:200,000.
After tooth extraction many patients planned dental implantation due to their young age. Moreover when third molar (wisdom) teeth are removed these areas of bone often become the site of autogenous bone fragments collection so it was necessary to perform the preservation of all removed teeth sockets.
Due to the fact that patients receiving antithrombotic therapy had a risk of developing early and delayed socket bleeding we decided to use collagen cones as an osteoplastic and hemostatic material. However closure of collagen cones with a mucous flap or a free graft could additionally provoke bleeding from the donor zone and therefore after atraumatic teeth extraction the edges of the mucosa above the socket brought together by simple sutures.
This technique was also used in comparison group patients.
The collagen cones of the Alvokon are easily inserted into the wound defect, quickly adapt to the walls of the alveoli and acquire the shape of the well of the removed tooth. Due to its hygroscopy the material swells rapidly creating compression of bone capillaries and small vessels.
The bleeding time from the removed tooth socket was recorded in all patients to assess the hemostatic properties of the material.
All patients underwent X-ray examinations of the area of interest immediately after removal and 1 month after to assess osteogenesis.
Results
The risk of bleeding in main group patients assessed by laboratory blood tests provided from medical outpatient records. After analyzing the hemostasis indicators: activated partial thromboplastin time (aPTT) and the lag-time before the beginning of accelerated thrombin production (LT) determined by the Hemker method slightly prolonged in all 17 patients who received selective inhibitors of blood clotting factor Xa (Table 1).
| Gender | Number of patient | Anticoagulant | aPTT | LT | |
| n | % | ||||
| Male | 4 | 23.5 | Rivaroxaban | Prolonged | Prolonged |
| 4 | 23.5 | Apixaban | Prolonged | Prolonged | |
| Female | 5 | 29 | Rivaroxaban | Prolonged | Prolonged |
| 4 | 24 | Apixaban | Prolonged | Prolonged | |
The assessment of bleeding time in patients of both groups was carried out on the basis of the formation of a blood clot in the socket after tooth extraction and the absence of blood leaks on a sterile napkin (Fig. 1).
The bleeding time in the main group varied from normal parameters (2—4 minutes) to prolonged. By gender prolonged bleeding time was revealed in all women of this group (Fig. 2) and only in men on Apixaban. In patients of the comparison group the formation of a stable blood clot in removed tooth socket regardless of gender took no more than 4 minutes (Table 2).
| Group | Gender | Number of patient | Anticoagulant | Bleeding time (minutes) | |
| n | % | ||||
| Main | Male | 4 | 23.5 | Rivaroxaban | 3—4 |
| 4 | 23.5 | Apixaban | 4—10 | ||
| Female | 5 | 29 | Rivaroxaban | 4—6 | |
| 4 | 23 | Apixaban | 5—15 | ||
| Comparison | Male | 5 | 50 | — | 2—4 |
| Female | 5 | 50 | — | 2—4 | |
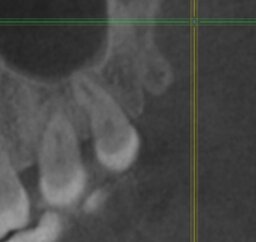
The effectiveness of osteogenesis in the area of the removed tooth after the use of collagen cones was evaluated based on a comparison of bone density on a CT scan in the area of interest made immediately after tooth extraction and 1 month after.
In both groups the density of the bone pattern in the area of interest increased which indicates normal osteogenesis. However in main group (Fig. 3) bone density was slightly lower than in comparison group (Fig. 4).
Discussion
Often patients with coronavirus infection SARS CoV-2 despite of their age are temporarily prescribed direct oral anticoagulants for thrombosis prevention [19, 20]. The reason for treatment of patients undergoing antiplatelet and anticoagulant therapy by dentist is an acute or exacerbation of chronic dental infection [16]. Removal of the infection source is recommended because odontogenic foci of infection increase the risk of vascular complications [9, 10, 23].
The functional activity of platelets increases under the influence of collagen. According to many authors direct anticoagulants of Xa factor despite the inhibition of thrombin formation platelet aggregation increases and their functional activity does not normalize [24].
In a study by Parfenyuk G.V. in 2021 all patients received oral anticoagulant Rivaroxaban and have increased in blood clotting time after tooth extraction even during using a hemostatics (pressure bandage with a swab moistened with tranexamic acid) [16]. In our study a blood clot was formed in the presence of an inducer of collagen platelet aggregation (collagen cones) to hold which the edges of the mucosa were brought together over the socket of the removed tooth. Prolongation of the bleeding time with this technique was observed only in women receiving Rivaroxaban which was 29% of the main group. In men on the same anticoagulant (23.5%) after socket curettage and filling with a collagen cone bleeding time was within normal limits as in the comparison group. The difference between our results and the study of Parfenyuk G.V. may be due to the age of the patients. Middle-aged patients were included in our study and elderly patients participated in the study of Parfenyuk G.V.
Interestingly that all patients who received Apixaban have prolonged formation of a blood clot with collagen cones and sutures to the edges of the mucosa. Perhaps this is due to the fact that Apixaban has a more pronounced effect of hypocoagulation and a lower degree of platelet aggregation induction.
For preserving the sockets of removed teeth the effectiveness of osteogenesis using collagen in combination with xenogenic bone powder is higher and described in some articles [13, 25—30]. However there are no articles in any database on the effectiveness of this method of preserving the sockets of removed teeth in patients on direct oral anticoagulants.
The results of the pilot study show the effectiveness of collagen cones not only as an osteoplastic material but also as an excellent local hemostatic.
Conclusion
Collagen cones are recommended for use in patients receiving antithrombotic therapy with selective inhibitors of blood clotting factors Xa in order to prevent the development of early and late local bleeding during surgical debridement of the oral cavity.
The osteoplastic properties of the collagen material are preserved even in patients receiving direct anticoagulants. It is necessary to continue studying the effect of collagen cones in combination with xenogenic bone fragments for preservation of dental socket and risk reduction of local hemorrhagic complications.
Clinical practice advices:
- When choosing the outer diameter of the collagen cone the inner socket diameter should be taken into account: if the socket is determined to be almost completely filled with Alvokon then it should be divided and 2/3 of the volume apply in the clot.
- Patient’s history should be carefully collected in order to avoid drug intolerance as hypersensitivity to the cones components: lidocaine and iodoform.
References
- Urban I.A., Monje A. Guided bone regeneration in alveolar bone reconstruction. Oral Maxillofac Surg Clin North Am. 2019; 31 (2): 331—8. PMID: 30947850
- Tolstunov L., Hamrick J.F.E., Broumand V., Shilo D., Rachmiel A. Bone Augmentation Techniques for Horizontal and Vertical Alveolar Ridge Deficiency in Oral Implantology. Oral Maxillofac Surg Clin North Am. 2019; 31 (2): 163—91. PMID: 30947846
- Buser D., Chappuis V., Belser U.C., Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late?. Periodontol 2000. 2017; 73 (1): 84—102. PMID: 28000278
- Wessing B., Lettner S., Zechner W. Guided Bone Regeneration with Collagen Membranes and Particulate Graft Materials: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018; 33 (1): 87—100. PMID: 28938035
- Liu Y., Sun X., Yu J., Wang J., Zhai P., Chen S., Liu M., Zhou Y. Platelet-rich fibrin as a bone graft material in oral and maxillofacial bone regeneration: Classification and summary for better application. Biomed Res Int. 2019; 2019: 3295756. PMID: 31886202
- Garcia J., Dodge A., Luepke P., Wang H.L., Kapila Y., Lin G.H. Effect of membrane exposure on guided bone regeneration: A systematic review and meta-analysis. Clin Oral Implants Res. 2018; 29 (3): 328—38. PMID: 29368353
- Shah F.A., Sayardoust S., Thomsen P., Palmquist A. Extracellular matrix composition during bone regeneration in the human dental alveolar socket. Bone. 2019; 127: 244—9. PMID: 31176735
- Solakoglu Ö., Heydecke G., Amiri N., Anitua E. The use of plasma rich in growth factors (PRGF) in guided tissue regeneration and guided bone regeneration. A review of histological, immunohistochemical, histomorphometrical, radiological and clinical results in humans. Ann Anat. 2020; 231: 151528. PMID: 32376297
- Giannobile W.V., Berglundh T., Al-Nawas B., Araujo M., Bartold P.M., Bouchard P., Chapple I., Gruber R., Lundberg P., Sculean A., Lang N.P., Lyngstadaas P., Kebschull M., Galindo-Moreno P., Schwartz Z., Shapira L., Stavropoulos A., Reseland J. Biological factors involved in alveolar bone regeneration: Consensus report of Working group 1 of the 15th European workshop on periodontology on bone regeneration. J Clin Periodontol. 2019; 46 Suppl 21: 6—11. PMID: 31215113
- Gruber R. Osteoimmunology: Inflammatory osteolysis and regeneration of the alveolar bone. J Clin Periodontol. 2019; 46 Suppl 21: 52—69. PMID: 30623453
- García-González S., Galve-Huertas A., Centenero S.A.H., Mareque-Bueno S., Satorres-Nieto M., Hernández-Alfaro F. Volumetric changes in alveolar ridge preservation with a compromised buccal wall: a systematic review and meta-analysis. Med Oral Patol Oral Cir Bucal. 2020; 25 (5): e565-e575. PMID: 32683381
- López-Pacheco A., Soto-Peñaloza D., Gómez M., Peñarrocha-Oltra D., Alarcón M.A. Socket seal surgery techniques in the esthetic zone: a systematic review with meta-analysis and trial sequential analysis of randomized clinical trials. Int J Implant Dent. 2021; 7 (1): 13. PMID: 33615421
- MacBeth N., Trullenque-Eriksson A., Donos N., Mardas N. Hard and soft tissue changes following alveolar ridge preservation: a systematic review. Clin Oral Implants Res. 2017; 28 (8): 982—1004. PMID: 27458031
- Ab T.K., T C.N., Ps G.D., Triveni M.G., Mehta D.S. A clinico-radiographic and histomorphometric analysis of alveolar ridge preservation using calcium phosphosilicate, PRF, and collagen plug. Maxillofac Plast Reconstr Surg. 2019; 41 (1): 32. PMID: 31523690
- Wiggins B.S., Dixon D.L., Neyens R.R., 2nd R.L.P., Gluckman T.J. Select drug-drug interactions with direct oral anticoagulants: JACC review topic of the week. J Am Coll Cardiol. 2020; 75 (11): 1341—50. PMID: 32192661
- Parfenyuk G.V. Dental and somatic components of the health of elderly patients undergoing prolonged therapy with new oral anticoagulants and optimization of outpatient surgical dental care: master’s thesis. Saratov, 2021. 152 p. (In Russ.).
- Velichko E.V.1, Khachukaeva A.S., Khabadze Z.S., Aksyonova E.M., Sturov N.V., Prokofeva E.B., Tedoradze R.V., Berisha A. Bemiparin in modern clinical practice. Difficult patient. 2017; 15 (10—11): 11—4 (In Russ.). eLIBRARY ID: 32399505
- Jonker B.P., Gil A., Naenni N., Jung R.E., Wolvius E.B., Pijpe J. Soft tissue contour and radiographic evaluation of ridge preservation in early implant placement: A randomized controlled clinical trial. Clin Oral Implants Res. 2021; 32 (1): 123—133. PMID: 33217058
- Arachchillage D.J., Remmington C., Rosenberg A., Xu T., Passariello M., Hall D., Laffan M., Patel B.V. Anticoagulation with argatroban in patients with acute antithrombin deficiency in severe COVID-19. Br J Haematol. 2020; 190 (5): e286-e288. PMID: 32516429
- Kipshidze N., Dangas G., White C.J., Kipshidze N., Siddiqui F., Lattimer C.R., Carter C.A., Fareed J. Viral coagulopathy in patients with COVID-19: Treatment and care. Clin Appl Thromb Hemost. 2020; 26: 1076029620936776. PMID: 32687449
- Yagyuu T., Kawakami M., Ueyama Y., Imada M., Kurihara M., Matsusue Y., Imai Y., Yamamoto K., Kirita T. Risks of postextraction bleeding after receiving direct oral anticoagulants or warfarin: a retrospective cohort study. BMJ Open. 2017; 7 (8): e015952. PMID: 28827248
- Caliskan M., Tükel H-C., Benlidayi M-E., Deniz A. Is it necessary to alter anticoagulation therapy for tooth extraction in patients taking direct oral anticoagulants?. Med Oral Patol Oral Cir Bucal. 2017; 22 (6): e767-e773. PMID: 29053656
- Thiem D.G.E., Polsak M., Römer P., Gielisch M., Blatt S., Al-Nawas B., Kämmerer P.W. The impact of the COVID-19 pandemic on the dental-maxillofacial emergency service of a German university hospital in the year 2020. Clin Oral Investig. 2021; 1—11. PMID: 34173887
- Geltser I.V. Features of anticoagulant action of rivaroxaban and laboratory control of its effectiveness: master‘s thesis abstract. Saint-Petersburg, 2018. 22 p. (In Russ.).
- Natto Z.S., Parashis A., Steffensen B., Ganguly R., Finkelman M.D., Jeong Y.N. Efficacy of collagen matrix seal and collagen sponge on ridge preservation in combination with bone allograft: A randomized controlled clinical trial. J Clin Periodontol. 2017; 44 (6): 649—659. PMID: 28303642
- Debel M., Toma S., Vandenberghe B., Brecx M.C., Lasserre J.F. Alveolar ridge dimensional changes after two socket sealing techniques. A pilot randomized clinical trial. Clin Oral Investig. 2021; 25 (3): 1235—1243. PMID: 32591869
- Testori T., Deflorian M.A., Mandelli F., Attardo G., Maiorana C., Fabbro M.D., Vinci R. Healing of Post-Extraction Sockets Filled with Anorganic Bovine Bone and Covered with a Xenogeneic Collagen Matrix. Radiological 2D and 3D Results of a Pilot Study to Assess Dimensional Stability. Materials (Basel). 2021; 14 (10): 2473. PMID: 34064679
- Yakovenko N.I., Vasil’ev Yu.L., Velichko E.V., Saleev R.A., Saleeva G.T. Clinical and radiological evaluation of the effectiveness of the use of collagen cones in the prevention of post-extraction complications. Clinical Dentistry (Russia). 2019; 4 (92): 74—7 (In Russ.). eLIBRARY ID: 41601790
- Castro A.B., Meschi N., Temmerman A., Pinto N., Lambrechts P., Teughels W., Quirynen M. Regenerative potential of leucocyte- and platelet-rich fibrin. Part B: sinus floor elevation, alveolar ridge preservation and implant therapy. A systematic review. J Clin Periodontol. 2017; 44 (2): 225—234. PMID: 27891638
- Zhou X., Yang J., Wu L., Tang X., Mou Y., Sun W., Hu Q., Xie S. Evaluation of the effect of implants placed in preserved sockets versus fresh sockets on tissue preservation and esthetics: A meta-analysis and systematic review. J Evid Based Dent Pract. 2019; 19 (4): 101336. PMID: 31843184