DOI:
10.37988/1811-153X_2021_1_108Protocols of digital diagnostics in patients with reduced lower third of the face
Downloads
Abstract
Determination of interalveolar height and centric relationship is a crucial problem in clinical dental practice, because possible failures lead to non-physiological position of mandible, which, in turn, can cause development of temporomandibular joint dysfunction and masticatory muscles disorders. The aim was to improve traditional protocol for determining interalveolar height and centric relationship in patients with reduced lower third of face.Materials and methods.
75 patients (27 men and 48 women) with tooth wear of II—III degree of severity and reduced lower third of face, suffered from pain, tension, fatigue, hypertension of masticatory muscles were examined. All patients were determined interalveolar height and centric relationship using the proposed method: first of all, instrumental diagnostics was performed (anatomico-instrumental method for determining interalveolar height and centric relationship with the help of gnathometer, created using special computer programs), and then the X-ray one (cone-beam computed tomography of temporomandibular joints with fixed together gnathometer’s bases in patient’s mouth). This method is described in clinical case.
Results.
It was achieved optimal condylar position and no pain in temporomandibular joints and masticatory muscles in the patient.
Conclusion.
Thus, high accuracy of diagnostics is achieved, due to the use of digital technologies at all clinical and laboratory stages.
Key words:
centric relationship, interalveolar height, reduced lower third of the face, teeth wear, digital diagnostics in dentistryFor Citation
Introduction
Determining the interalveolar height and centric relationship of jaws (CRJ) is a crucial problem in clinical prosthodontics [1—11]. Failures on their determining lead to a non-physiological position of condyle, which, in turn, may cause the development of temporomandibular joint dysfunction (TMJ) and masticatory muscle disorders [12—22]. Inducing the digital diagnostic methods into dental practice allows to improve the previously proposed methods for determining the interalveolar height and CRJ, which improves considerably the quality of treatment [23—29].
Objective. Improving the traditional protocol of determining the interalveolar height and centric relation of jaws in patients with reduced lower third of the face.
Materials and methods
75 patients (27 men and 48 women) aged 21 to 65 (average age 33.3±5.7) were examined. The criteria for inclusion in the study were patients with excessive tooth abrasion of II-III degree of severity and reduced lower third of the face with intact dentitions, as well as dentitions with Kennedy I-III Class defects, suffering from pain, tension, fatigue, hypertension of masticatory muscles for over 1 month duration.
The criteria for non-inclusion were patients with chronic generalized periodontitis of moderate or severe degree, persons with a surgical intervention in anamnesis (arthroscopy, arthrocentesis), TMJ traumas, systemic inflammatory TMJ diseases (rheumatoid arthritis), and patients having been treated for masticatory muscle hypertension during the last 6 months.
The control group included 31 people in good health (9 men, 22 women) aged 16 to 31 (average age 27.8±3.2) with intact dentitions and orthognathic bite. The interalveolar height and the CRJ was estimated by anatomic-instrumental method (using the intraoral recording device — gnathometer) in all patients of the basic group.
The technology of creating the gnathometers was fully implemented upon the digital protocol: the first stage included optical impressions of the upper and lower jaws using the intraoral scanner Medit i500 (South Korea), than the modelling of gnathometer was performed by the software Exocad DentalCAD (Germany) and after its completion the finished product was manufactured with 3D printer FormLabs Form2 (USA).
Checking the position of TMJ condyle after determining the interalveolar height and CRJ followed using our method offered — by means of a radiological investigation. That is, first of all the instrumental diagnostics was carried out (anatomic-instrumental way of determining the interalveolar height and CRJ) and after that the radiological one (cone-beam computer tomography of TMJ with apparatus bases of the upper and lower jaws of the intraoral recording device fixed together in the patient's mouth). Thus, the checking of topography of the temporomandibular joint condyle reduces considerably their dislocation from the normal position.
The radiological investigation was performed using the cone-beam computer tomograph “KaVo 3D eXam” (KaVo Dental, Germany). The received tomograms were analyzed by InVivo 5 Anatomage software. The articular fossa in sagittal plane was calculated with the method offered by K. Ikeda и A. Kawamura (2009) [30].
Clinical case
Patient K., 51 years of age, went to the dental clinic of the Galaxy Beauty Institute (Saint Petersburg, Russia) with complaints of fatigue of the masticatory muscles, clenching the teeth, increased tooth wear, feeling of stuffiness in the ears, reduced lower portion of the face, pronounced nasolabial folds, drooping corners of the mouth.
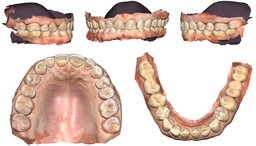
The external inspection revealed a decreased size of the lower face portion, deepened nasolabial and mental folds. The degree of mouth opening was 45 mm, palpation of masticatory muscles painless. The inspection of the oral cavity showed some semilunar shape erasure edges on the masticatory tooth surfaces of the upper and the lower jaws, chipped ceramic facets of artificial crowns (Fig. 1).
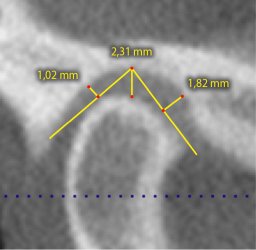
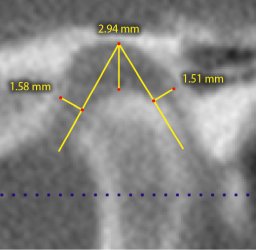
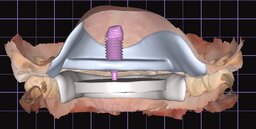
The estimation of the cone-beam computer tomogram (the patient had received it already) allowed to set the dimensions of the articular gap at right in the frontal portion 1.82 mm, in the upper one 2.31 mm, in the posterior 1.02 mm; at left in front 1.58 mm, in the upper part 2.32 mm, posteriorly 1.51 mm. So, the posterior position of condyle in the central occlusion was revealed, which could indicate a forced position of the mandible (Fig. 2).
Based on clinical and paraclinical investigation methods the following was diagnosed: Bruxism (F45.82), Increased abrasion of the teeth (K03.0).
An extended diagnostic plan was drawn up: 1) taking the optic impressions from the upper and lower dentitions; 2) creating the intraoral recording device; 3) studying the biomechanics of the lower jaw, determination of the interalveolar height and the CRJ by means of gnathometer.
Taking the optic impressions from the upper and lower jaws was carried out using the intraoral scanner (Fig. 3). The received optical scans were saved in the STL format and transferred to the dental laboratory.
After that the device bases and gnathometer tables were modelled by the dental technician using the Exocad DentalCAD software. Creation of the intraoral recording device was performed in the “Occlusal splint” module. First the device basis of the lower jaw was modelled: they opened the «Border» tab and with the help of a computer mouse cursor, the boundaries of the basis were drawn along the points, the undercuts corrected, the sharp edges smoothed out. Then on this basis the intraoral device table was formed: shape and parameters (radius, width, height) of the geometric object, which form the table, one can select it in the program library.
Similarly, the device basis and the table of the upper dentition were modeled where the hole for the writing pin was formed (its diameter had been measured before and made 3.5 mm). Preliminary the writing pin was scanned, the received virtual prototype was loaded into the library of the program Exocad DentalCAD, and after that the pin was positioned in the hole formed on the upper table. The virtual writing pin was saved in the library of Exocad DentalCAD program and is used when creating new gnathometers (Fig. 4).
Thus, one table serves for fixing the records of the lower jaw movement in three mutually perpendicular planes, the other one for fixing the writing pin into it.
Upon modelling completion, the intraoral recording device was produced on the 3D printer (laser stereolithography). The substrate for 3D printing was the FormLabs photopolymer resin. After printing, the models were cleansed in a special automatic cleaning device Formlabs Form Wash and then processed in the UV curing unit Formlabs Form Cure to provide a uniform hardening the photopolymer resin.
At the next clinical appointment, the interalveolar height and CRJ were determined by the offered method, as well as the biomechanics of mandibular movements was explored (Fig. 5).
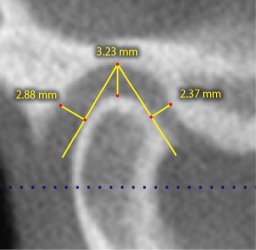
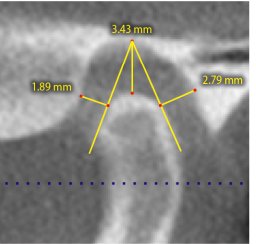
After finding the interalveolar height and CRJ the gnathometer bases of the upper and lower jaws were fixed together in the oral cavity by means of silicone material Bisico Regidur (Germany), and the patient was referred to the X-ray room. The results of CBCT with gnathometer in the oral cavity sowed a central (physiological) position of the temporomandibular joint condyles in the articular fossae. The joint space sizes showed at right in the front section 2.37 mm, 3.23 mm in the upper and 2.88 in the posterior one; at left in the front section 1.89 mm, 3.43 mm in the upper and 2.79 mm in the posterior section (Fig. 6).
After the radiological checkup the intraoral recording device was removed from the oral cavity, the bases of the upper and lower jaw were kept bonded together. Then the dental laboratory operator scanned the gnathometer using the scanner ZirkonZahn (Italy). In the virtual articulator Amann Girrbach of the Exocad DentalCad software the dental technician oriented the optical impressions of the patient's dentitions taking into consideration the data received by means of gnathometer and then started creating the splint. The appliance was made by milling by means of ZirkonZahn CAD/CAM System equipment. The made splint allowed to save the found position of the mandible at the preparatory stage of complex treatment of the patient (Fig. 7).
Conclusion
Thus, using the anatomical and instrumental method of determining the interalveolar height and centric relationship of jaws combined with cone-beam computer tomography makes possible, firstly, to improve the detection accuracy of interalveolar height and CRJ; secondly, to check the topography of condylar position, which significantly reduces the risk of TMJ and masticatory muscle dysfunction development.
Figures

References
- Trezubov V.N., Chikunov S.O., Bulycheva E.A., Alpat‘eva Ju.V., Bulycheva D.S. Step by step modeling of dentiton in difficult clinical picture. — Clinical Dentistry (Russia). — 2017; 3(83): 60—3 (In Russ.).
- Guguvcevski L., Gigovski N., Mijoska A., Zlatanovska K., Arsova-Gigovska A. Temporomandibular disorders treatment with correction of decreased occlusal vertical dimension. — Open Access Maced J Med Sci. — 2017; 5 (7): 983—6. PMID: 29362632
- Abolmasov N.N., Prygunov K.A., Abolmasov N.G., Adaeva I.A. Assessment of occlusive and articulatory dentition interrelation in determination of etiological factors and symptoms of various pathological conditions. — The Dental Institute. — 2018; 1 (78): 62—3 (In Russ.).
- Stafeev A.A., Ryakhovsky A.N., Petrov P.O., Chikunov S.O., Khizhuk A.V. A comparative analysis of reproducibility of the jaws centric relation determined with the use of digital technologies. — Stomatology. — 2019; 6 (98): 83—9 (In Russ.).
- Kandasamy S., Greene C.S., Obrez A. An evidence-based evaluation of the concept of centric relation in the 21st century. — Quintessence Int. — 2018; 49 (9): 755—760. PMID: 30202837
- Koretskaya E.A., Kalmin O.V., Zyul'kina L.A., Ivanov P.V. Characteristics of elasticity of of solid tissue of teeth (literature review). — University Proceedings. Volga region. Medical sciences. — 2018; 3 (47): 141—56 (In Russ.).
- Vagner V.D., Bulycheva E.A. The quality of dental care: characteristics and criteria. — Stomatology. — 2017; 1 (96): 23—4 (In Russ.).
- Wiens J.P., Goldstein G.R., Andrawis M., Choi M., Priebe J.W. Defining centric relation. — J Prosthet Dent. — 2018; 120 (1): 114—22. PMID: 29526300
- The glossary of prosthodontic terms: Ninth Edition. — J Prosthet Dent. — 2017; 117 (5S): e1-e105. PMID: 28418832
- Goldstein G., Andrawis M., Choi M., Wiens J., Janal M.N. A survey to determine agreement regarding the definition of centric relation. — J Prosthet Dent. — 2017; 117 (3): 426—9. PMID: 27765398
- Palaskar J.N., Murali R., Bansal S. Centric relation definition: a historical and contemporary prosthodontic perspective. — J Indian Prosthodont Soc. — 2013; 13 (3): 149—54. PMID: 24431728
- de Kanter R.J.A.M., Battistuzzi P.G.F.C.M., Truin G.-J. Temporomandibular disorders: "Occlusion" matters! — Pain Res Manag. — 2018; 8746858. PMID: 29861806
- Ponomarev A.V., Postnikov M.A., Trunin D.A. Estimation of the effectiveness in prosthodontic treatment of temporomandibular joint dysfunction according to mathematical modeling. — Dentist. — 2018; 1 (28): 96—102 (In Russ.).
- Wiens J.P., Priebe J.W. Occlusal stability. — Dent Clin North Am. — 2014; 58 (1): 19—43. PMID: 24286644
- Ohrbach R., Dworkin S.F. The evolution of TMD diagnosis: Past, present, future. — J Dent Res. — 2016; 95 (10): 1093—101. PMID: 27313164
- Lövgren A., Häggman-Henrikson B., Visscher C.M., Lobbezoo F., Marklund S., Wänman A. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan—A population based study. — Eur J Pain. — 2016; 20 (4): 532—40. PMID: 26311138
- Rajapakse S., Ahmed N., Sidebottom A.J. Current thinking about the management of dysfunction of the temporomandibular joint: a review. — Br J Oral Maxillofac Surg. — 2017; 55 (4): 351—6. PMID: 28341275
- Chisnoiu A.M., Picos A.M., Popa S., Chisnoiu P.D., Lascu L., Picos A., Chisnoiu R. Factors involved in the etiology of temporomandibular disorders — a literature review. — Clujul Med. — 2015; 88 (4): 473—8. PMID: 26732121
- Postnikov M.A., Nesterov A.M., Trunin D.A., Sadykov M.I., Gabdrafikov R.R., Sagirov M.R. Possibilities of diagnostics and complex treatment of patients with TMJ disfunctions. — Clinical Dentistry (Russia). — 2020; 1 (93): 60—3 (In Russ.).
- Mikhaylova V.V., Voityazkaya I.V., Kaspina A.I. Trophic disorders and pain symptoms in the maxillofacial region in patients with dentition defects, accompanied by a decrease in interalveolar distance. State of the problem. — The Dental Institute. — 2014; 3 (64): 86—7 (In Russ.).
- Murphy M.K., MacBarb R.F., Wong M.E., Athanasiou K.A. Temporomandibular disorders: a review of etiology, clinical management, and tissue engineering strategies. — Int J Oral Maxillofac Implants. — 2013; 28 (6): e393—414. PMID: 24278954
- Durham J., Newton-John T.R.O., Zakrzewska J.M. Temporomandibular disorders. — BMJ. — 2015; 350: h1154. PMID: 25767130
- Kim J.-E., Park J.-H., Moon H.-S., Shim J.-S. Complete assessment of occlusal dynamics and establishment of a digital workflow by using target tracking with a three-dimensional facial scanner. — J Prosthodont Res. — 2019; 63 (1): 120—4. PMID: 30446410
- Trezubov V.N., Bulycheva E.A., Lobko Yu.V., Davydenko D.D., Brechov A.A., Bulycheva D.S. Planning and implementation of prosthodontics using digital technologies in patients with complete tooth loss. — Digital Dentistry. — 2017; 1 (6): 4—13. (In Russ.).
- Gvetadze R.S., Timofeev D.E., Butova V.G., Jerebcov A.Yu., Andreeva S.N. Additive digital technologies in dentistry. — Russian Journal of Dentistry. — 2018; 5 (22): 224—8 (In Russ.).
- Ryakhovsky A.N., Boytsova E.A. 3D analysis of the temporomandibular joint and occlusal relationships based on computer virtual simulation. — Stomatology. — 2020; 2 (99): 97—104 (In Russ.).
- Zhulev E.N., Vokulova Yu.A. Evaluation of the dimensional accuracy of the artificial crowns' frames from lithium disilicate made using traditional and digital technologies. — Dental Forum. — 2020; 3 (78): 27—33 (In Russ.).
- Zande M.M., Gorter R.C., Bruers J.J.M., Aartman I.H.A., Wismeijer D. Dentists' opinions on using digital technologies in dental practice. — Community Dent Oral Epidemiol. — 2018; 46 (2): 143—153. PMID: 28983942
- Steinmassl P.-A., Klaunzer F., Steinmassl O., Dumfahrt H., Grunert I. Evaluation of currently available CAD/CAM denture systems. — Int J Prosthodont. — 2017; 30 (2): 116—22. PMID: 28267817
- Ikeda K., Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. — Am J Orthod Dentofacial Orthop. — 2009; 135 (4): 495—501. PMID: 19361736